H5N1 influenza is evolving rapidly, weakening the effectiveness of existing antibodies and increasing its potential threat to humans.
Scientists at UNC Charlotte and MIT used high-performance computational modeling to analyze thousands of viral protein-antibody interactions, revealing a decline in immune response effectiveness. Their research suggests that H5N1 mutations may soon enable human-to-human transmission, raising pandemic concerns. The virus has already spread among wild birds, poultry, cattle, and even farmworkers, emphasizing the need for swift vaccine development.
H5N1's Rapid Evolution Poses a Growing Threat
A research team at the University of North Carolina at Charlotte has used advanced computational modeling to study how the H5N1 bird flu virus interacts with the immune system. Their findings show that the virus is evolving in ways that help it evade immune defenses, whether from past infection or vaccination, in mammals.
Published on March 17 in eBioMedicine (a journal within The Lancet family), the study highlights urgent concerns. As avian influenza continues to spread globally, it poses not only a serious risk to agriculture but also an increasing threat to human health.
Worsening Antibody Affinity Raises Concerns
The researchers found a clear trend: antibodies are becoming less effective against newer strains of H5N1. This "worsening antibody affinity" suggests that future versions of the virus may be even more difficult for the immune system to recognize and fight, raising the risk of transmission to and among humans.
The study's lead author is Colby T. Ford, Ph.D., a visiting scholar in data science at UNC Charlotte's CIPHER center and founder of Tuple, LLC, a biotechnology consulting firm based in Charlotte.
Crucially, Ford explains, this rapid adaptation means that "if one makes an H5N1 vaccine with a previous vaccine candidate virus, the vaccine will have less efficacy, based on our measurements of how much the virus has evolved in recent years" As such, the team's research approach provides guidance for keeping pace with a rapidly adapting viral threat.
The team from UNC Charlotte's Department of Bioinformatics and Genomics includes students Shirish Yasa, Khaled Obeid, and Sayal Guirales-Medrano, led by Bioinformatics Assistant Professor Richard Allen White III, Ph.D., and CIPHER Co-Director Daniel Janies, Ph.D. who is the Carol Grotnes Belk Distinguished Professor of Bioinformatics and Genomics. The UNC Charlotte team collaborated with researchers from the Massachusetts Institute of Technology: Rafael Jaimes III, Ph.D., and Phillip J. Tomezsko, Ph.D.
Antigenic Drift and Increased Zoonotic Risk
By examining the virus' rampant host-shifting and recent mutations comprehensively, researchers find "the continuous transmission of H5N1 from birds to mammals and the increase in strains with immuno-evasive HA in mammals sampled over time suggest that antigenic drift is a source of zoonotic risk."
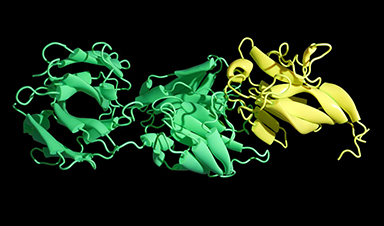
In the paper, "Large-scale computational modeling of H5 influenza variants against HA1-neutralising antibodies," the UNC Charlotte research team shares their results from analysis of 1,804 viral protein-host antibody comparisons. The experiments consisted of current hemagglutinin domain 1 viral proteins computationally bound in physics models to neutralizing antibodies obtained from infected hosts and vaccine recipients from 1996 to 2018.
Computational Modeling Reveals Alarming Trends
Using high-performance computational modeling, CIPHER researchers documented "a trend of weakening binding affinity of a wide variety of existing antibodies, collected from vaccinated and or infected hosts, against H5 viral isolates over time."
Due to the public health importance, the findings were available via preprint publication in July 2024 prior to successful peer review. Due to the computational tools they had assembled during the SARS-CoV-2 pandemic, the team was able to complete this work on H5N1 just three months after the first reported cow-to-human transmission of H5N1, which was reported in a farmworker in Texas.
In assessing the possible pandemic risk spurred by H5 bird flu spread and mutation, global researchers agree that "the avian virus (remains) high on lists of potential pandemic agents," as reported in Science in December 2024.
H5N1 Cases Surge in Mammals and Poultry
As of this writing, no human-to-human transmission has been reported. However, cattle in at least 17 states have tested positive for H5N1 in addition to millions of cases among wild birds, small mammals, commercial chickens, and other flocks. Between January 2022 and March 2025, the Centers for Disease Control reported:
- 12,510 outbreaks among wild birds in the U.S.
- 51 jurisdictions with bird flu among wild birds.
- 166,417,923 poultry affected
- 70 human cases of H5N1, one fatal, in the U.S.
The H5N1 virus, according to the World Health Organization, has killed 466 people worldwide since January 2003.
Speed Crucial to Combat a Fast-Adapting Virus
Vaccines, many experts say, will likely be a crucial tool in controlling a bird flu pandemic, as mutations of viral lineages adapt to new mammal hosts.
In eBioMedicine, the research team from Charlotte writes that their findings "indicate that the virus has potential to move from epidemic to pandemic status in the near future."
The study – along with other research that confirms worsening antibody binding over time alongside increased avian-to-mammalian transmission – indicates "there is an impending danger to human health for highly pathogenic strains of H5 influenza that can infect avian and mammalian livestock and jump to humans."
Avian Influenza can already be considered a pandemic among wild and domesticated animals due to the virus' pervasive spread across geography and species. Likewise, the spread of H5N1 from wild birds to chickens, dairy cattle, and farm workers illustrates the opportunism of infections across species.
Now, UNC Charlotte's computational modeling results "specifically assert that the worsening trend of the antibody performance along with the already present animal pandemic is a cause for concern for an eventual human pandemic."
Computational Modeling: A Key Tool for Preparedness
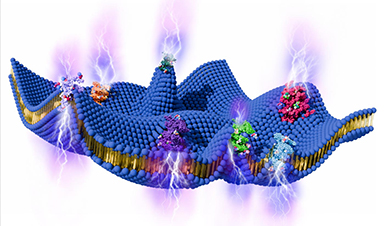
Further, the authors write that high-performance computing – which in this case included AI-based protein folding and physics-based simulations of viral protein-antibody interactions – provides rapid and reliable results to inform leaders in preparedness.
Janies, in a recent interview, explained the utility of computational modeling as a means of understanding viral mutation as well as predictive thinking concerning how a virus is evolving.
High-performance computational modeling, Janies said, is a pathway for "chipping away at multiple angles of biological variation at speed and scale" to "tune our intuition to the right approaches" for vaccine efficacy and infection control as viruses evolve.
Reference: "Large-scale computational modelling of H5 influenza variants against HA1-neutralising antibodies" by Colby T. Ford, Shirish Yasa, Khaled Obeid, Rafael Jaimes, Phillip J. Tomezsko, Sayal Guirales-Medrano, Richard Allen White and Daniel Janies, 17 March 2025, eBioMedicine.
DOI: 10.1016/j.ebiom.2025.105632
The protein modeling research on H5N1 viral lineages conducted at UNC Charlotte was funded by an Ignite grant from the UNC Charlotte Division of Research. Research used genetic data and metadata from GISAID, the Global Initiative on Sharing All Influenza Data, and the United States National Institutes of Health's GenBank.
News
The Brain’s Strange Way of Computing Could Explain Consciousness
Consciousness may emerge not from code, but from the way living brains physically compute. Discussions about consciousness often stall between two deeply rooted viewpoints. One is computational functionalism, which holds that cognition can be [...]
First breathing ‘lung-on-chip’ developed using genetically identical cells
Researchers at the Francis Crick Institute and AlveoliX have developed the first human lung-on-chip model using stem cells taken from only one person. These chips simulate breathing motions and lung disease in an individual, [...]
Cell Membranes May Act Like Tiny Power Generators
Living cells may generate electricity through the natural motion of their membranes. These fast electrical signals could play a role in how cells communicate and sense their surroundings. Scientists have proposed a new theoretical [...]
This Viral RNA Structure Could Lead to a Universal Antiviral Drug
Researchers identify a shared RNA-protein interaction that could lead to broad-spectrum antiviral treatments for enteroviruses. A new study from the University of Maryland, Baltimore County (UMBC), published in Nature Communications, explains how enteroviruses begin reproducing [...]
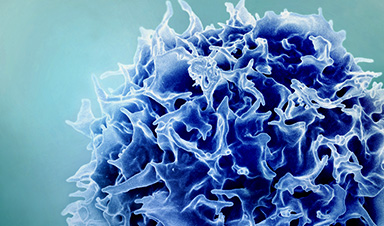
New study suggests a way to rejuvenate the immune system
Stimulating the liver to produce some of the signals of the thymus can reverse age-related declines in T-cell populations and enhance response to vaccination. As people age, their immune system function declines. T cell [...]
Nerve Damage Can Disrupt Immunity Across the Entire Body
A single nerve injury can quietly reshape the immune system across the entire body. Preclinical research from McGill University suggests that nerve injuries may lead to long-lasting changes in the immune system, and these [...]
Fake Science Is Growing Faster Than Legitimate Research, New Study Warns
New research reveals organized networks linking paper mills, intermediaries, and compromised academic journals Organized scientific fraud is becoming increasingly common, ranging from fabricated research to the buying and selling of authorship and citations, according [...]
Scientists Unlock a New Way to Hear the Brain’s Hidden Language
Scientists can finally hear the brain’s quietest messages—unlocking the hidden code behind how neurons think, decide, and remember. Scientists have created a new protein that can capture the incoming chemical signals received by brain [...]
Does being infected or vaccinated first influence COVID-19 immunity?
A new study analyzing the immune response to COVID-19 in a Catalan cohort of health workers sheds light on an important question: does it matter whether a person was first infected or first vaccinated? [...]
We May Never Know if AI Is Conscious, Says Cambridge Philosopher
As claims about conscious AI grow louder, a Cambridge philosopher argues that we lack the evidence to know whether machines can truly be conscious, let alone morally significant. A philosopher at the University of [...]
AI Helped Scientists Stop a Virus With One Tiny Change
Using AI, researchers identified one tiny molecular interaction that viruses need to infect cells. Disrupting it stopped the virus before infection could begin. Washington State University scientists have uncovered a method to interfere with a key [...]
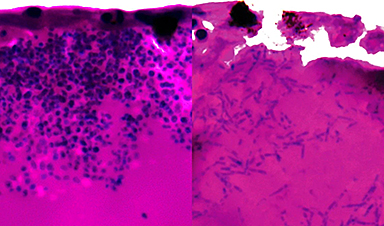
Deadly Hospital Fungus May Finally Have a Weakness
A deadly, drug-resistant hospital fungus may finally have a weakness—and scientists think they’ve found it. Researchers have identified a genetic process that could open the door to new treatments for a dangerous fungal infection [...]
Fever-Proof Bird Flu Variant Could Fuel the Next Pandemic
Bird flu viruses present a significant risk to humans because they can continue replicating at temperatures higher than a typical fever. Fever is one of the body’s main tools for slowing or stopping viral [...]
What could the future of nanoscience look like?
Society has a lot to thank for nanoscience. From improved health monitoring to reducing the size of electronics, scientists’ ability to delve deeper and better understand chemistry at the nanoscale has opened up numerous [...]
Scientists Melt Cancer’s Hidden “Power Hubs” and Stop Tumor Growth
Researchers discovered that in a rare kidney cancer, RNA builds droplet-like hubs that act as growth control centers inside tumor cells. By engineering a molecular switch to dissolve these hubs, they were able to halt cancer [...]
Platelet-inspired nanoparticles could improve treatment of inflammatory diseases
Scientists have developed platelet-inspired nanoparticles that deliver anti-inflammatory drugs directly to brain-computer interface implants, doubling their effectiveness. Scientists have found a way to improve the performance of brain-computer interface (BCI) electrodes by delivering anti-inflammatory drugs directly [...]