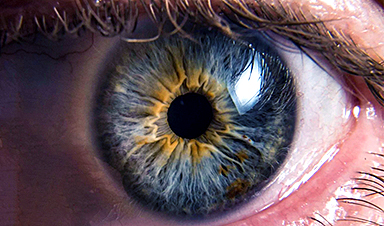
Blocking the PROX1 protein allowed KAIST researchers to regenerate damaged retinas and restore vision in mice.
Vision is one of the most important human senses, yet more than 300 million people around the world are at risk of losing it due to various retinal diseases. Although recent treatments have helped slow the progression of these conditions, no effective therapy has been able to restore vision that has already been lost, until now. Researchers at KAIST have developed a new drug that successfully restores vision.
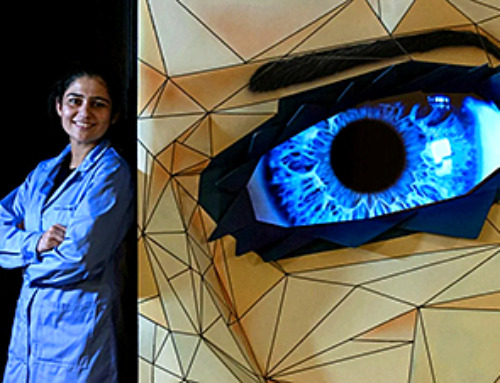
On March 30, KAIST announced that a research team headed by Professor Jin Woo Kim from the Department of Biological Sciences has created a treatment that regenerates retinal nerves to restore vision.

In experiments using a disease-model mouse, the team achieved both retinal regeneration and vision recovery by blocking the PROX1 (prospero homeobox 1) protein, which normally prevents retinal repair. The results were long-lasting, with effects continuing for more than six months.
First long-term retinal repair in mammals
This study marks the first successful induction of long-term neural regeneration in mammalian retinas, offering new hope to patients with degenerative retinal diseases who previously had no treatment options.
As the global population continues to age, the number of retinal disease patients is steadily increasing. However, no treatments exist to restore damaged retinas and vision. The primary reason for this is the mammalian retina’s inability to regenerate once damaged.

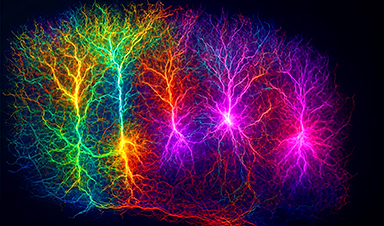
Studies on cold-blooded animals, such as fish—known for their robust retinal regeneration—have shown that retinal injuries trigger Müller glia cells to dedifferentiate into retinal progenitor cells, which then generate new neurons. However, in mammals, this process is impaired, leading to permanent retinal damage.
PROX1 protein identified as a regeneration blocker
Through this study, the research team identified the PROX1 protein as a key inhibitor of Müller glia dedifferentiation in mammals. PROX1 is a protein found in neurons of the retina, hippocampus, and spinal cord, where it suppresses neural stem cell proliferation and promotes differentiation into neurons.
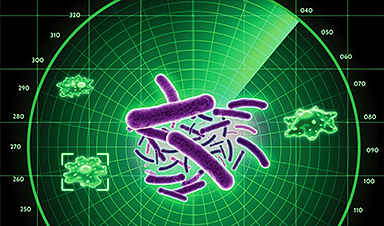
The researchers discovered that PROX1 accumulates in damaged mouse retinal Müller glia, but is absent in the highly regenerative Müller glia of fish. Furthermore, they demonstrated that the PROX1 found in Müller glia is not synthesized internally but rather taken up from surrounding neurons, which fail to degrade and instead secrete the protein.

Based on this finding, the team developed a method to restore Müller glia’s regenerative ability by eliminating extracellular PROX1 before it reaches these cells.
This approach involves using an antibody that binds to PROX1, developed by Celliaz Inc., a biotech startup founded by Professor Jin Woo Kim’s research lab. When administered to disease-model mouse retinas, this antibody significantly promoted neural regeneration. Additionally, when delivered, the antibody gene to the retinas of retinitis pigmentosa disease model mice, it enabled sustained retinal regeneration and vision restoration for over six months.
The retinal regeneration-inducing therapy is currently being developed by Celliaz Inc. for application in various degenerative retinal diseases that currently lack effective treatments. The company aims to begin clinical trials by 2028.
Dr. Eun Jung Lee stated, “We are about to complete the optimization of the PROX1-neutralizing antibody (CLZ001) and move to preclinical studies before administering it to retinal disease patients. Our goal is to provide a solution for patients at risk of blindness who currently lack proper treatment options.”
Reference: “Restoration of retinal regenerative potential of Müller glia by disrupting intercellular Prox1 transfer” by Eun Jung Lee, Museong Kim, Sooyeon Park, Ji Hyeon Shim, Hyun-Ju Cho, Jung Ah Park, Kihyun Park, Dongeun Lee, Jeong Hwan Kim, Haeun Jeong, Fumio Matsuzaki, Seon-Young Kim, Jaehoon Kim, Hanseul Yang, Jeong-Soo Lee and Jin Woo Kim, 25 March 2025, Nature Communications.
DOI: 10.1038/s41467-025-58290-8
This research was supported by research funds from the Korean National Research Foundation (NRF) and the Korea Drug Development Foundation (KDDF).