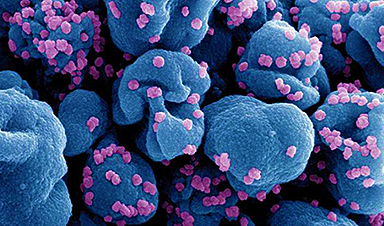
Nanomedicine, a branch of nanotechnology, is revolutionizing healthcare by enabling the manipulation of materials at the nanoscale to diagnose, treat, and prevent diseases.
Unlike traditional treatments, nanoparticles (NPs) are highly precise in targeting diseased cells at the molecular level, enhancing the effectiveness of treatments for conditions like cancer, diabetes, infectious diseases, chronic pain, and autoimmune diseases. This precision also minimizes treatment side effects, reshaping modern medicine, particularly in the context of antibiotic resistance.
As nanomedicine evolves, ethical considerations surrounding its development and application are gaining attention from the global health community. Key concerns include assessing and managing the risks associated with engineered NPs and ensuring clear communication of these risks during clinical trials.
Beyond safety, ethical issues such as patient privacy, data security, and equitable treatment access remain pressing challenges. Researchers and practitioners are responsible for addressing these concerns as regulatory frameworks struggle to keep pace with technological advancements.
Privacy: Data Security and Patient Consent
Nanomedicine often depends on the collection and analysis of large amounts of personal data, including genetic information, to achieve statistically sound conclusions and tailor treatments to individual patients. However, this extensive data collection presents significant risks if not adequately protected, making privacy and data security critical to maintaining trust in the field.
Patient consent is a key aspect of privacy, especially as nanomedical devices become more advanced and increasingly integrated with artificial intelligence and machine learning. These advancements raise concerns about the devices’ growing capacity to generate and process patient data.
Therefore, obtaining informed consent from patients is crucial in nanomedicine, where data usage has far-reaching consequences. Researchers and medical practitioners must communicate clearly with patients regarding how their data will be used, stored, and transferred before they agree to participate in nanomedicine treatments or research.
Safety: Long-Term Effects and Regulatory Standards
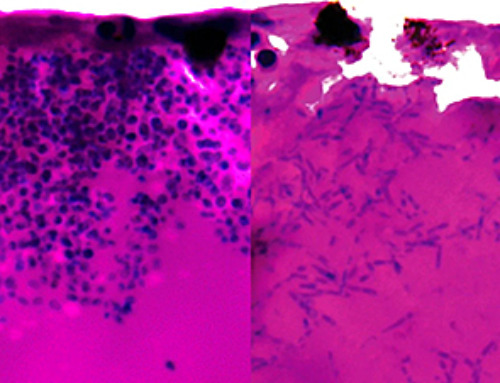
Nanomedicine raises major ethical concerns regarding toxicity, especially since the long-term effects of using NPs in the human body are not yet fully understood by medical practitioners.
NPs possess intricate physical and chemical traits, such as their composition, structure, size, surface features, porosity, charge, and stability. These properties can vary widely, making it challenging to define NPs for specific treatments.
Polydispersity, which refers to variations in particle size, shape, or mass, is a crucial characteristic of NPs that differentiates them from other chemicals. Even among NPs of the same average size, variations in polydispersity can significantly impact secondary properties like targeting efficiency, drug release rates, biocompatibility, toxicity, and in vivo behavior.
Therefore, comprehensive studies are essential to evaluate the potential risks of nanomedicine, including long-term toxicity and interactions with other biological systems that could cause unwanted side effects.
While regulatory standards are vital for ensuring the safety of any medical practice, existing regulations may not be fully equipped to address the unique challenges nanotechnology poses. It is imperative for regulatory authorities to understand, establish, and enforce standard practices for testing, approval, and monitoring to minimize the risks associated with using NPs in the medical field.
Equity: Access to Nanomedicine Treatments
Access to nanomedicine presents a significant ethical issue, particularly concerning equity. Like many advanced medical technologies, nanomedicine has the potential to widen existing disparities in healthcare access. The high costs and limited availability of sophisticated infrastructure could create substantial barriers for patients in low-income or marginalized communities, preventing them from accessing nanomedicine treatments.
Developed countries, including the US, Canada, Germany, and South Korea, dominate NP research, leading to a global imbalance in access to nanomedical technology. Meanwhile, people in developing countries often face challenges accessing these treatments.
It is crucial to explore ways to make nanomedicine accessible to all patients worldwide, regardless of socioeconomic status, and to ensure inclusivity in research on the effects of such medications across different ethnic groups.
One approach to addressing these economic disparities is implementing global policies aimed at making treatments more affordable and providing financial assistance to low-income patients. Additionally, investing in healthcare infrastructure in underprivileged regions would help ensure that everyone has access to the benefits of nanomedicine.
Transparency: Clear Communication of Risks and Benefits
Effectively communicating the risks associated with nanotechnology to research subjects and the broader public is a significant challenge. Strict guidelines require that participants be provided with detailed information about the purpose, procedures, benefits, risks, and confidentiality measures of the research study, including for medical treatments involving nanomedicine. This ensures that participants can make informed decisions about their involvement.
However, studies indicate that research subjects often underestimate the risks and overestimate the benefits of participation. Additionally, they may not fully understand that the primary goal of clinical studies is to generate knowledge that could benefit future patients, rather than to provide optimal care for current participants.
Building trust in nanomedicine depends on providing patients and the public with clear, accurate, and accessible information about the methods, potential side effects, and likelihood of success for each specific treatment. Establishing transparency and open dialogue standards is essential for fostering confidence in these emerging treatment methods.
Accountability: Responsibility of Researchers and Practitioners
Accountability is a key ethical consideration in nanomedicine. Researchers and medical practitioners have a duty to ensure that the development, testing, and use of nanomedicine always prioritize the patient’s safety. Respecting patient rights and adhering to ethical standards is of utmost importance. This includes conducting rigorous testing, obtaining informed consent, and being transparent about potential risks.
Accountability also extends to the broader societal impact of nanomedicine, such as the long-term implications of the work. The effect of new nanomedicines and related practices on public health, the environment, and social structure has to be considered by everybody working in the field.4 Nanomedicine professionals require a commitment to responsible innovation, where the benefits of nanomedicine are maximized and potential harm is minimized.
Summary and Future Directions
NPs have significantly advanced clinical medicine, particularly in therapeutics and diagnostics. Innovations such as stealth and long-circulating liposomes have become established in clinical applications, as highlighted in a study published in Materials Science and Engineering: C.
However, despite these advancements, nanomedicine is still in its early stages and faces several challenges before it can achieve widespread approval. As the field evolves, it is vital to prioritize ethical considerations in research, policy, and clinical practice to unlock its full potential while protecting patient rights.
Nanomedicine products must demonstrate favorable pharmacological and safety profiles, as well as efficacy in clinical trials. Early collaboration among large pharmaceutical companies, smaller firms, and researchers from diverse disciplines—from nanotechnology to medicine—should be encouraged during preclinical development to leverage the strengths of each partner.
Integrating resources from academia, industry, consortia, and hospitals is essential for connecting nanomedicine’s physicochemical properties with its biological effects. Health authorities must also develop clear definitions, quality standards, and regulatory guidelines specific to nanomedicine.
Given its complexity, nanomedicine presents unique challenges in controlling processes and monitoring biological behavior. However, these challenges can be addressed with systematic and rational approaches, enabling nanomedicine to make significant contributions to medicine and healthcare.
News
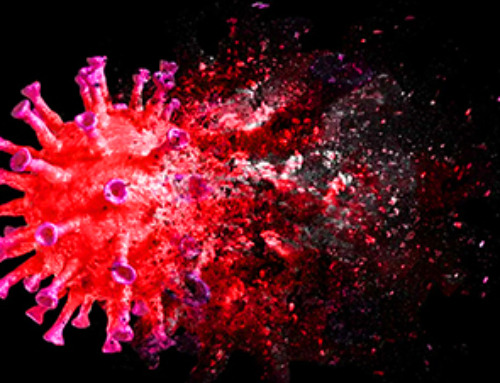
Does being infected or vaccinated first influence COVID-19 immunity?
A new study analyzing the immune response to COVID-19 in a Catalan cohort of health workers sheds light on an important question: does it matter whether a person was first infected or first vaccinated? [...]
We May Never Know if AI Is Conscious, Says Cambridge Philosopher
As claims about conscious AI grow louder, a Cambridge philosopher argues that we lack the evidence to know whether machines can truly be conscious, let alone morally significant. A philosopher at the University of [...]
AI Helped Scientists Stop a Virus With One Tiny Change
Using AI, researchers identified one tiny molecular interaction that viruses need to infect cells. Disrupting it stopped the virus before infection could begin. Washington State University scientists have uncovered a method to interfere with a key [...]
Deadly Hospital Fungus May Finally Have a Weakness
A deadly, drug-resistant hospital fungus may finally have a weakness—and scientists think they’ve found it. Researchers have identified a genetic process that could open the door to new treatments for a dangerous fungal infection [...]
Fever-Proof Bird Flu Variant Could Fuel the Next Pandemic
Bird flu viruses present a significant risk to humans because they can continue replicating at temperatures higher than a typical fever. Fever is one of the body’s main tools for slowing or stopping viral [...]
What could the future of nanoscience look like?
Society has a lot to thank for nanoscience. From improved health monitoring to reducing the size of electronics, scientists’ ability to delve deeper and better understand chemistry at the nanoscale has opened up numerous [...]
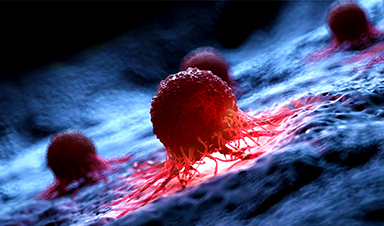
Scientists Melt Cancer’s Hidden “Power Hubs” and Stop Tumor Growth
Researchers discovered that in a rare kidney cancer, RNA builds droplet-like hubs that act as growth control centers inside tumor cells. By engineering a molecular switch to dissolve these hubs, they were able to halt cancer [...]
Platelet-inspired nanoparticles could improve treatment of inflammatory diseases
Scientists have developed platelet-inspired nanoparticles that deliver anti-inflammatory drugs directly to brain-computer interface implants, doubling their effectiveness. Scientists have found a way to improve the performance of brain-computer interface (BCI) electrodes by delivering anti-inflammatory drugs directly [...]
After 150 years, a new chapter in cancer therapy is finally beginning
For decades, researchers have been looking for ways to destroy cancer cells in a targeted manner without further weakening the body. But for many patients whose immune system is severely impaired by chemotherapy or radiation, [...]
Older chemical libraries show promise for fighting resistant strains of COVID-19 virus
SARS‑CoV‑2, the virus that causes COVID-19, continues to mutate, with some newer strains becoming less responsive to current antiviral treatments like Paxlovid. Now, University of California San Diego scientists and an international team of [...]
Lower doses of immunotherapy for skin cancer give better results, study suggests
According to a new study, lower doses of approved immunotherapy for malignant melanoma can give better results against tumors, while reducing side effects. This is reported by researchers at Karolinska Institutet in the Journal of the National [...]
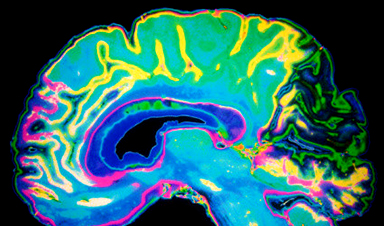
Researchers highlight five pathways through which microplastics can harm the brain
Microplastics could be fueling neurodegenerative diseases like Alzheimer's and Parkinson's, with a new study highlighting five ways microplastics can trigger inflammation and damage in the brain. More than 57 million people live with dementia, [...]
Tiny Metal Nanodots Obliterate Cancer Cells While Largely Sparing Healthy Tissue
Scientists have developed tiny metal-oxide particles that push cancer cells past their stress limits while sparing healthy tissue. An international team led by RMIT University has developed tiny particles called nanodots, crafted from a metallic compound, [...]
Gold Nanoclusters Could Supercharge Quantum Computers
Researchers found that gold “super atoms” can behave like the atoms in top-tier quantum systems—only far easier to scale. These tiny clusters can be customized at the molecular level, offering a powerful, tunable foundation [...]
A single shot of HPV vaccine may be enough to fight cervical cancer, study finds
WASHINGTON -- A single HPV vaccination appears just as effective as two doses at preventing the viral infection that causes cervical cancer, researchers reported Wednesday. HPV, or human papillomavirus, is very common and spread [...]
New technique overcomes technological barrier in 3D brain imaging
Scientists at the Swiss Light Source SLS have succeeded in mapping a piece of brain tissue in 3D at unprecedented resolution using X-rays, non-destructively. The breakthrough overcomes a long-standing technological barrier that had limited [...]