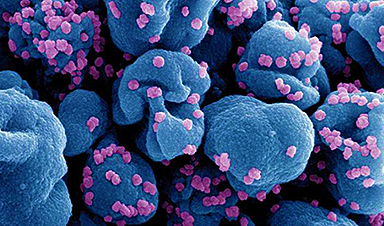
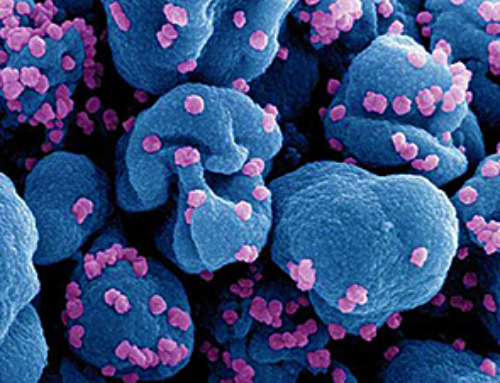
A research team from Johns Hopkins Medicine and Johns Hopkins University has developed a machine-learning (ML) tool capable of predicting who has the highest probability of being naturally resistant to COVID-19 infection despite being exposed to SARS-CoV-2, the virus that causes it.
The study, published this week in PLOS One, aims to better understand the factors that influence COVID-19 resistance.
“If we can identify which people are naturally able to avoid infection by SARS-CoV-2, we may be able to learn — in addition to societal and behavioral factors — which genetic and environmental differences influence their defense against the virus,” said Karen (Kai-Wen) Yang, lead study author and a biomedical engineering graduate student in the Translational Informatics Research and Innovation Lab at Johns Hopkins University, in the press release. “That insight could lead to new preventive measures and more highly targeted treatments.”
To develop their model, the researchers gathered data from the Johns Hopkins COVID-19 Precision Medicine Analytics Platform Registry (JH-CROWN), which contains information for patients with a suspected or confirmed SARS-CoV-2 infection seen within the Johns Hopkins Health System, the press release states.
From this information, the research team selected patients who had received a COVID-19 test between June 10, 2020, and Dec. 15, 2020, and reported “potential exposure to the virus” as the reason for testing. Dec. 15 was chosen as the end date because it was just before large-scale COVID-19 vaccination efforts began in the US, which allowed researchers to avoid the confounding effects of vaccines, rather than natural resistance, on preventing COVID-19 infection.
The final cohort comprised 8,536 study participants who were divided into two groups: those who either did not share a household with any COVID-19 patients or whose household had 10 or more patients, and those who shared a residence with 10 or fewer people, with at least one being a COVID-19 patient.
The first group, consisting of 8,476 participants, served as the training and initial testing test, while the remaining 60 participants were grouped into a Household Index (HHI) Set, which served as a separate testing set.
EHR data from the cohort was analyzed using the Maximal-frequent All-confident pattern Selection Pattern-based Clustering (MASPC) algorithm, which combines patient demographic information, the relevant International Statistical Classification of Diseases and Related Health Problems (ICD) medical diagnostic codes, outpatient medication orders, and the number of comorbidities present for each patient.
“We hypothesized that MASPC would enable us to cluster patients with similar patterns in their data to define them as resistant and non-resistant to SARS-CoV-2, and with the hope that the algorithm would learn with each analysis how to improve the accuracy and reliability of future assignments,” explained co-senior study author Stuart Ray, MD, vice chair of medicine for data integrity and analytics, and professor of medicine at the Johns Hopkins University School of Medicine, in the press release. “This initial study using JH-CROWN data was conducted to give life to that hypothesis, a proof-of-concept trial of our statistical model to show that resistance to COVID-19 might be predictable based [on] a patient’s clinical and demographic profile.”
The researchers were able to identify 56 of these patterns, five of which captured who was most likely exposed to the virus.
“Looking for these patterns in HHI Set — the individuals most likely to have been exposed to SARS-CoV-2 in close quarters — and then statistically analyzing the results, our model’s best performance was 0.61,” says Ray. “Since a score of 0.5 shows only chance association between the prediction and reality, and 1 is 100% association, this shows the model has promise as a tool for identifying people with COVID-19 resistance who can be further studied.”
The researchers noted that the study has multiple limitations, such as potential bias from the self-reporting of COVID-19 exposure by participants, the small number of participants in the HHI group, the short timeframe of the study, and the possibility that participants may have taken tests for SARS-CoV-2 using home kits or at facilities outside the Johns Hopkins system, which would not have been recorded in the JH-CROWN database.
News
Platelet-inspired nanoparticles could improve treatment of inflammatory diseases
Scientists have developed platelet-inspired nanoparticles that deliver anti-inflammatory drugs directly to brain-computer interface implants, doubling their effectiveness. Scientists have found a way to improve the performance of brain-computer interface (BCI) electrodes by delivering anti-inflammatory drugs directly [...]
After 150 years, a new chapter in cancer therapy is finally beginning
For decades, researchers have been looking for ways to destroy cancer cells in a targeted manner without further weakening the body. But for many patients whose immune system is severely impaired by chemotherapy or radiation, [...]
Older chemical libraries show promise for fighting resistant strains of COVID-19 virus
SARS‑CoV‑2, the virus that causes COVID-19, continues to mutate, with some newer strains becoming less responsive to current antiviral treatments like Paxlovid. Now, University of California San Diego scientists and an international team of [...]
Lower doses of immunotherapy for skin cancer give better results, study suggests
According to a new study, lower doses of approved immunotherapy for malignant melanoma can give better results against tumors, while reducing side effects. This is reported by researchers at Karolinska Institutet in the Journal of the National [...]
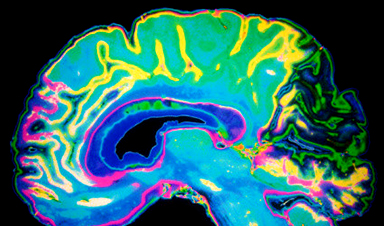
Researchers highlight five pathways through which microplastics can harm the brain
Microplastics could be fueling neurodegenerative diseases like Alzheimer's and Parkinson's, with a new study highlighting five ways microplastics can trigger inflammation and damage in the brain. More than 57 million people live with dementia, [...]
Tiny Metal Nanodots Obliterate Cancer Cells While Largely Sparing Healthy Tissue
Scientists have developed tiny metal-oxide particles that push cancer cells past their stress limits while sparing healthy tissue. An international team led by RMIT University has developed tiny particles called nanodots, crafted from a metallic compound, [...]
Gold Nanoclusters Could Supercharge Quantum Computers
Researchers found that gold “super atoms” can behave like the atoms in top-tier quantum systems—only far easier to scale. These tiny clusters can be customized at the molecular level, offering a powerful, tunable foundation [...]
A single shot of HPV vaccine may be enough to fight cervical cancer, study finds
WASHINGTON -- A single HPV vaccination appears just as effective as two doses at preventing the viral infection that causes cervical cancer, researchers reported Wednesday. HPV, or human papillomavirus, is very common and spread [...]
New technique overcomes technological barrier in 3D brain imaging
Scientists at the Swiss Light Source SLS have succeeded in mapping a piece of brain tissue in 3D at unprecedented resolution using X-rays, non-destructively. The breakthrough overcomes a long-standing technological barrier that had limited [...]
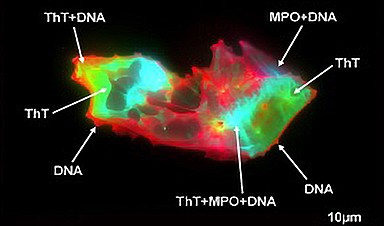
Scientists Uncover Hidden Blood Pattern in Long COVID
Researchers found persistent microclot and NET structures in Long COVID blood that may explain long-lasting symptoms. Researchers examining Long COVID have identified a structural connection between circulating microclots and neutrophil extracellular traps (NETs). The [...]
This Cellular Trick Helps Cancer Spread, but Could Also Stop It
Groups of normal cbiells can sense far into their surroundings, helping explain cancer cell migration. Understanding this ability could lead to new ways to limit tumor spread. The tale of the princess and the [...]
New mRNA therapy targets drug-resistant pneumonia
Bacteria that multiply on surfaces are a major headache in health care when they gain a foothold on, for example, implants or in catheters. Researchers at Chalmers University of Technology in Sweden have found [...]
Current Heart Health Guidelines Are Failing To Catch a Deadly Genetic Killer
New research reveals that standard screening misses most people with a common inherited cholesterol disorder. A Mayo Clinic study reports that current genetic screening guidelines overlook most people who have familial hypercholesterolemia, an inherited disorder that [...]
Scientists Identify the Evolutionary “Purpose” of Consciousness
Summary: Researchers at Ruhr University Bochum explore why consciousness evolved and why different species developed it in distinct ways. By comparing humans with birds, they show that complex awareness may arise through different neural architectures yet [...]
Novel mRNA therapy curbs antibiotic-resistant infections in preclinical lung models
Researchers at the Icahn School of Medicine at Mount Sinai and collaborators have reported early success with a novel mRNA-based therapy designed to combat antibiotic-resistant bacteria. The findings, published in Nature Biotechnology, show that in [...]
New skin-permeable polymer delivers insulin without needles
A breakthrough zwitterionic polymer slips through the skin’s toughest barriers, carrying insulin deep into tissue and normalizing blood sugar, offering patients a painless alternative to daily injections. A recent study published in the journal Nature examines [...]