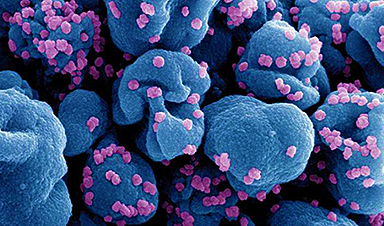
Long COVID, affecting 5-10% of COVID-19 patients, might be caused by the enduring presence of the virus in the body.
Research suggests that viral fragments, possibly live, linger and lead to symptoms. Addressing this involves antiviral treatments, enhanced public awareness, and preventive measures against reinfection.
Understanding Long COVID and Its Prevalence
About 5–10% of people infected with COVID-19 develop long COVID, experiencing symptoms that last three months or longer.
Scientists have suggested several biological mechanisms to explain long COVID. However, in a recent perspective article in the Medical Journal of Australia, we propose that long COVID may largely be caused by the virus itself persisting in the body.
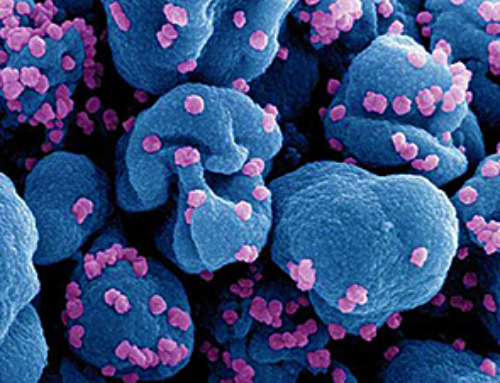
Since the early days of the pandemic, researchers have recognized that SARS-CoV-2 — or its remnants — can remain in different tissues and organs long after the initial infection. This phenomenon is referred to as "viral persistence."
Credit: SciTechDaily.com
Evidence of Persistent Virus and Its Implications
While the long-term presence of residual viral fragments in some people's bodies is now well established, what remains less certain is whether live virus itself, not just old bits of virus, is lingering – and if so, whether this is what causes long COVID. This distinction is crucial because live virus can be targeted by specific antiviral approaches in ways that "dead" viral fragments cannot.
Viral persistence has two significant implications:
- when it occurs in some highly immunocompromised people, it is thought to be the source of new and substantially different-looking variants, such as JN.1
- it has the potential to continue to cause symptoms in many people in the wider population long beyond the acute illness. In other words, long COVID could be caused by a long infection.
Current Research Findings on Viral Persistence
While there remains no single study that confirms that persistent virus is the cause of long COVID, collectively several recent key papers make a compelling case.
In February, a study in Nature found a high number of people with mild COVID symptoms had extended periods of shedding the genetic material of the virus, so-called viral RNA, from their respiratory tract. Those with persistent shedding of this viral RNA – which almost certainly represents the presence of live virus – were at higher risk of long COVID.
Other key papers detected replicating viral RNA and proteins in blood fluid of patients years after their initial infection, a sign that the virus is likely replicating for long periods in some hidden reservoirs in the body, perhaps including blood cells.
Another study detected viral RNA in ten different tissue sites and blood samples 1–4 months after acute infection. This study found the risk of long COVID (measured four months following infection) was higher in those with persistently positive viral RNA.
The same study also gave clues about where in the body the persisting virus resides. The gastrointestinal tract is one site of considerable interest as a long-term viral hideout.
The Challenge of Proving Viral Replication
Earlier this month, further evidence of persistent virus increasing likelihood of long COVID has been published as part of the RECOVER initiative, a collaborative research project that aims to address the impacts of long COVID.
However, formal proof that virus capable of replicating can last for years in the body remains elusive. This is because isolating the live virus from reservoirs inside the body where the virus "hides" is technically challenging.
In its absence, we and other scientists argue the cumulative evidence is now sufficiently compelling to galvanise action.
Strategies to Address Long COVID
The obvious response to this is to fast-track trials of known antivirals for prevention and cure of long COVID.
This should include more left-field therapies such as the diabetes drug metformin. This has possible dual benefits in the context of long COVID:
- its antiviral properties, which have demonstrated surprising efficacy against long COVID
- as a potential therapeutic in treating impairments related to fatigue.
However, another major thrust should be the development of new drugs and the establishment of clinical trial platforms for rapid testing.
Science has uncovered exciting therapeutic options. But translating these into forms usable in the clinic is a large hurdle that requires support and investment from governments.
Raising Awareness and Preventing Long COVID
The notion of "long infection" as a contributor or even the driver of long COVID is a powerful message. It could help demystify the condition in the eyes of the wider community and increase awareness among the general public as well as medical professionals.
It should help raise awareness in the community of the importance of reducing rates of re-infection. It is not just your first infection, but each subsequent COVID infection carries a risk of long COVID.
Long COVID is common and isn't restricted to those at high risk of severe acute disease but affects all age groups. In one study, the highest impact was in those aged 30 to 49 years.
Preventive Measures and Future Outlook
So, for now, we all need to reduce our exposure to the virus with the tools available, a combination of:
- clean indoor air approaches. In its simplest form, this means being conscious of the importance of well-ventilated indoor spaces, opening the windows and improving airflow as COVID spreads through air. More sophisticated ways of ensuring indoor air is safe involve monitoring quality and filtering air in spaces that cannot be easily naturally ventilated
- using high-quality masks (that are well-fitting and don't let air in easily, such as N95-type masks) in settings where you don't have confidence of the quality of the indoor air and/or that are crowded
- testing, so you know when you're positive. Then, if you're eligible, you can get treatment. And you can be vigilant about protecting those around you with masks, staying at home where possible, and ventilating spaces
- staying up to date with COVID booster doses. Vaccines reduce long COVID and other post-COVID complications.
Hopefully one day there will be better treatments and even a cure for long COVID. But in the meantime, increased awareness of the biomedical basis of long COVID should prompt clinicians to take patients more seriously as they attempt to access the treatments and services that already exist.
Written by:
- Brendan Crabb, Director and CEO, Burnet Institute
- Gabriela Khoury, Theme Leader, Antiviral Immunity, Burnet Institute
- Michelle Scoullar, Senior Research Fellow, Burnet Institute
Adapted from an article originally published in The Conversation.
News
Scientists Melt Cancer’s Hidden “Power Hubs” and Stop Tumor Growth
Researchers discovered that in a rare kidney cancer, RNA builds droplet-like hubs that act as growth control centers inside tumor cells. By engineering a molecular switch to dissolve these hubs, they were able to halt cancer [...]
Platelet-inspired nanoparticles could improve treatment of inflammatory diseases
Scientists have developed platelet-inspired nanoparticles that deliver anti-inflammatory drugs directly to brain-computer interface implants, doubling their effectiveness. Scientists have found a way to improve the performance of brain-computer interface (BCI) electrodes by delivering anti-inflammatory drugs directly [...]
After 150 years, a new chapter in cancer therapy is finally beginning
For decades, researchers have been looking for ways to destroy cancer cells in a targeted manner without further weakening the body. But for many patients whose immune system is severely impaired by chemotherapy or radiation, [...]
Older chemical libraries show promise for fighting resistant strains of COVID-19 virus
SARS‑CoV‑2, the virus that causes COVID-19, continues to mutate, with some newer strains becoming less responsive to current antiviral treatments like Paxlovid. Now, University of California San Diego scientists and an international team of [...]
Lower doses of immunotherapy for skin cancer give better results, study suggests
According to a new study, lower doses of approved immunotherapy for malignant melanoma can give better results against tumors, while reducing side effects. This is reported by researchers at Karolinska Institutet in the Journal of the National [...]
Researchers highlight five pathways through which microplastics can harm the brain
Microplastics could be fueling neurodegenerative diseases like Alzheimer's and Parkinson's, with a new study highlighting five ways microplastics can trigger inflammation and damage in the brain. More than 57 million people live with dementia, [...]
Tiny Metal Nanodots Obliterate Cancer Cells While Largely Sparing Healthy Tissue
Scientists have developed tiny metal-oxide particles that push cancer cells past their stress limits while sparing healthy tissue. An international team led by RMIT University has developed tiny particles called nanodots, crafted from a metallic compound, [...]
Gold Nanoclusters Could Supercharge Quantum Computers
Researchers found that gold “super atoms” can behave like the atoms in top-tier quantum systems—only far easier to scale. These tiny clusters can be customized at the molecular level, offering a powerful, tunable foundation [...]
A single shot of HPV vaccine may be enough to fight cervical cancer, study finds
WASHINGTON -- A single HPV vaccination appears just as effective as two doses at preventing the viral infection that causes cervical cancer, researchers reported Wednesday. HPV, or human papillomavirus, is very common and spread [...]
New technique overcomes technological barrier in 3D brain imaging
Scientists at the Swiss Light Source SLS have succeeded in mapping a piece of brain tissue in 3D at unprecedented resolution using X-rays, non-destructively. The breakthrough overcomes a long-standing technological barrier that had limited [...]
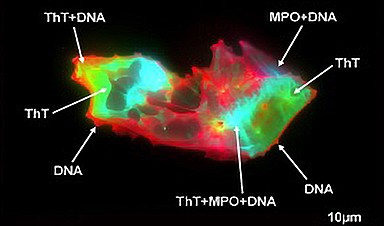
Scientists Uncover Hidden Blood Pattern in Long COVID
Researchers found persistent microclot and NET structures in Long COVID blood that may explain long-lasting symptoms. Researchers examining Long COVID have identified a structural connection between circulating microclots and neutrophil extracellular traps (NETs). The [...]
This Cellular Trick Helps Cancer Spread, but Could Also Stop It
Groups of normal cbiells can sense far into their surroundings, helping explain cancer cell migration. Understanding this ability could lead to new ways to limit tumor spread. The tale of the princess and the [...]
New mRNA therapy targets drug-resistant pneumonia
Bacteria that multiply on surfaces are a major headache in health care when they gain a foothold on, for example, implants or in catheters. Researchers at Chalmers University of Technology in Sweden have found [...]
Current Heart Health Guidelines Are Failing To Catch a Deadly Genetic Killer
New research reveals that standard screening misses most people with a common inherited cholesterol disorder. A Mayo Clinic study reports that current genetic screening guidelines overlook most people who have familial hypercholesterolemia, an inherited disorder that [...]
Scientists Identify the Evolutionary “Purpose” of Consciousness
Summary: Researchers at Ruhr University Bochum explore why consciousness evolved and why different species developed it in distinct ways. By comparing humans with birds, they show that complex awareness may arise through different neural architectures yet [...]
Novel mRNA therapy curbs antibiotic-resistant infections in preclinical lung models
Researchers at the Icahn School of Medicine at Mount Sinai and collaborators have reported early success with a novel mRNA-based therapy designed to combat antibiotic-resistant bacteria. The findings, published in Nature Biotechnology, show that in [...]