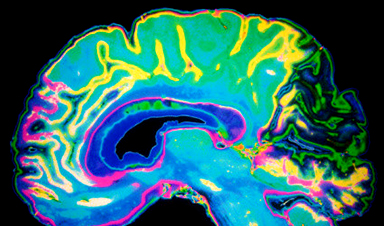
New method uses patient-derived neurons to effectively simulate late-onset Alzheimer's and identify possible treatments.
Researchers at Washington University School of Medicine in St. Louis have created a technique to explore the impact of aging on Alzheimer's disease development. This new method allows for the study of aged neurons in the laboratory without requiring a brain biopsy, which could enhance understanding of the disease and lead to novel treatment approaches.
The scientists transformed skin cells taken from patients with late-onset Alzheimer's disease into brain cells called neurons. Late-onset Alzheimer's develops gradually over many decades and only starts to show symptoms at age 65 or older. For the first time, these lab-derived neurons accurately reproduced the hallmarks of this type of dementia, including the amyloid beta buildup, tau protein deposits, and neuronal cell death.
By studying these cells, the researchers identified aspects of cells' genomes — called retrotransposable elements, which change their activity as we age — in the development of late-onset Alzheimer's disease. The findings suggest new treatment strategies targeting these factors.
The study appears Aug. 2 in the journal Science.
Challenges in Alzheimer's Research
"Sporadic, late-onset Alzheimer's disease is the most common type of Alzheimer's disease, representing more than 95% of cases," said senior author Andrew Yoo, PhD, a professor of developmental biology. "It has been very difficult to study in the lab due to the complexity of the disease stemming from various risk factors, including aging as an important contributor. Until now, we did not have a way to capture the effects of aging in the cells to study late-onset Alzheimer's."

To date, animal studies of Alzheimer's disease have, by necessity, focused on mice with rare genetic mutations known to cause inherited, early-onset Alzheimer's in younger people — a strategy that has shed light on the condition but differs from disease development for the vast majority of patients with the sporadic, late-onset form. To more faithfully recapitulate the disease in the lab, Yoo's team turned to an approach called cellular reprogramming.
The method to transform easily obtained human skin cells from living patients directly into neurons makes it possible to study Alzheimer's effects on the brain without the risk of a brain biopsy and in a way that retains the consequences of the patient's age on the neurons. Past work by Yoo and his colleagues, who pioneered this transformation technique using small RNA molecules called microRNAs, has focused on understanding the development of Huntington's disease — an inherited neurological condition that typically shows adult-onset symptoms.
Observations from Neuronal Spheroids
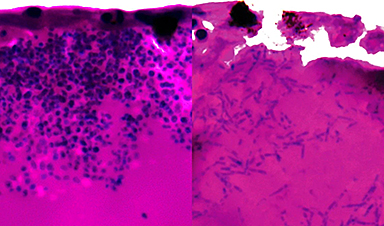
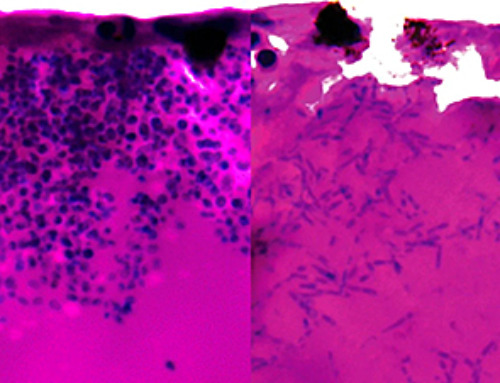
After transforming skin cells into brain cells, the researchers found that the new neurons can grow in a thin gel layer or self-assemble into small clusters — called spheroids — mimicking the 3D environment of the brain. The researchers compared neuronal spheroids generated from patients with sporadic, late-onset Alzheimer's disease, inherited Alzheimer's disease, and healthy individuals of similar ages.
The Alzheimer's disease patients' spheroids quickly developed amyloid beta deposits and tau tangles between neurons. Activation of genes associated with inflammation also emerged, and then the neurons began to die, mimicking what is seen in brain scans of patients. Spheroids from older, healthy donors in the study showed some amyloid deposition but much less than those from patients. The small amyloid deposits in older, healthy spheroids are evidence that the technique is capturing the effects of age and suggests that amyloid beta and tau accumulation correlated with aging. It further demonstrates that the Alzheimer's disease process makes the buildup far worse.
The researchers, including first author Zhao Sun, PhD, a staff scientist in Yoo's lab, found that treating spheroids from late-onset Alzheimer's disease patients with drugs that interfere with the formation of amyloid beta plaques early in the disease process, before neurons start forming toxic amyloid beta buildup, significantly reduced the amyloid beta deposits. But treating at later time points, after some buildup was already present, had no effect or only modestly reduced subsequent amyloid beta deposits. Such data emphasize the importance of identifying and treating the disease early.
Role of Genetic Elements in Alzheimer's
The study further found a role for retrotransposable elements — small pieces of DNA that jump to different locations in the genome — in the development of late-onset Alzheimer's disease. Inhibition of such "jumping genes" with the drug lamivudine (also called 3TC) — an anti-retroviral drug that can dampen the activity of retrotransposable elements — had a positive effect: The spheroids from late-onset Alzheimer's disease patients had reduced amyloid beta and tau tangles and showed less neuronal death compared with the same spheroids treated with a placebo. Lamivudine treatment had no beneficial effect on spheroids from patients with early-onset, inherited Alzheimer's disease, providing evidence that sporadic late-onset Alzheimer's development related to aging has distinct molecular features compared with inherited autosomal dominant Alzheimer's disease.
"In these patients, our new model system has identified a role for retrotransposable elements associated with the disease process," Yoo said. "We were pleased to see that we could reduce the damage with a drug treatment that suppresses these elements. We look forward to using this model system as we work toward new personalized therapeutic interventions for late-onset Alzheimer's disease."
The researchers are planning future studies with spheroids that include multiple types of brain cells, including neurons and glia.
Reference: "Modeling late-onset Alzheimer's disease neuropathology via direct neuronal reprogramming" by Zhao Sun, Ji-Sun Kwon, Yudong Ren, Shawei Chen, Courtney K. Walker, Xinguo Lu, Kitra Cates, Hande Karahan, Sanja Sviben, James A. J. Fitzpatrick, Clarissa Valdez, Henry Houlden, Celeste M. Karch, Randall J. Bateman, Chihiro Sato, Steven J. Mennerick, Marc I. Diamond, Jungsu Kim, Rudolph E. Tanzi, David M. Holtzman and Andrew S. Yoo, 2 August 2024, Science.
DOI: 10.1126/science.adl2992
The study was funded by the Farrell Family Foundation, the Cure Alzheimer's Fund, the Centene Corporation, Edward Mallinckrodt, Washington University NeuroGenomics and Informatics Center, the Children's Discovery Institute, the Foundation for Barnes-Jewish Hospital, and the National Institutes of Health.
News
Does being infected or vaccinated first influence COVID-19 immunity?
A new study analyzing the immune response to COVID-19 in a Catalan cohort of health workers sheds light on an important question: does it matter whether a person was first infected or first vaccinated? [...]
We May Never Know if AI Is Conscious, Says Cambridge Philosopher
As claims about conscious AI grow louder, a Cambridge philosopher argues that we lack the evidence to know whether machines can truly be conscious, let alone morally significant. A philosopher at the University of [...]
AI Helped Scientists Stop a Virus With One Tiny Change
Using AI, researchers identified one tiny molecular interaction that viruses need to infect cells. Disrupting it stopped the virus before infection could begin. Washington State University scientists have uncovered a method to interfere with a key [...]
Deadly Hospital Fungus May Finally Have a Weakness
A deadly, drug-resistant hospital fungus may finally have a weakness—and scientists think they’ve found it. Researchers have identified a genetic process that could open the door to new treatments for a dangerous fungal infection [...]
Fever-Proof Bird Flu Variant Could Fuel the Next Pandemic
Bird flu viruses present a significant risk to humans because they can continue replicating at temperatures higher than a typical fever. Fever is one of the body’s main tools for slowing or stopping viral [...]
What could the future of nanoscience look like?
Society has a lot to thank for nanoscience. From improved health monitoring to reducing the size of electronics, scientists’ ability to delve deeper and better understand chemistry at the nanoscale has opened up numerous [...]
Scientists Melt Cancer’s Hidden “Power Hubs” and Stop Tumor Growth
Researchers discovered that in a rare kidney cancer, RNA builds droplet-like hubs that act as growth control centers inside tumor cells. By engineering a molecular switch to dissolve these hubs, they were able to halt cancer [...]
Platelet-inspired nanoparticles could improve treatment of inflammatory diseases
Scientists have developed platelet-inspired nanoparticles that deliver anti-inflammatory drugs directly to brain-computer interface implants, doubling their effectiveness. Scientists have found a way to improve the performance of brain-computer interface (BCI) electrodes by delivering anti-inflammatory drugs directly [...]
After 150 years, a new chapter in cancer therapy is finally beginning
For decades, researchers have been looking for ways to destroy cancer cells in a targeted manner without further weakening the body. But for many patients whose immune system is severely impaired by chemotherapy or radiation, [...]
Older chemical libraries show promise for fighting resistant strains of COVID-19 virus
SARS‑CoV‑2, the virus that causes COVID-19, continues to mutate, with some newer strains becoming less responsive to current antiviral treatments like Paxlovid. Now, University of California San Diego scientists and an international team of [...]
Lower doses of immunotherapy for skin cancer give better results, study suggests
According to a new study, lower doses of approved immunotherapy for malignant melanoma can give better results against tumors, while reducing side effects. This is reported by researchers at Karolinska Institutet in the Journal of the National [...]
Researchers highlight five pathways through which microplastics can harm the brain
Microplastics could be fueling neurodegenerative diseases like Alzheimer's and Parkinson's, with a new study highlighting five ways microplastics can trigger inflammation and damage in the brain. More than 57 million people live with dementia, [...]
Tiny Metal Nanodots Obliterate Cancer Cells While Largely Sparing Healthy Tissue
Scientists have developed tiny metal-oxide particles that push cancer cells past their stress limits while sparing healthy tissue. An international team led by RMIT University has developed tiny particles called nanodots, crafted from a metallic compound, [...]
Gold Nanoclusters Could Supercharge Quantum Computers
Researchers found that gold “super atoms” can behave like the atoms in top-tier quantum systems—only far easier to scale. These tiny clusters can be customized at the molecular level, offering a powerful, tunable foundation [...]
A single shot of HPV vaccine may be enough to fight cervical cancer, study finds
WASHINGTON -- A single HPV vaccination appears just as effective as two doses at preventing the viral infection that causes cervical cancer, researchers reported Wednesday. HPV, or human papillomavirus, is very common and spread [...]
New technique overcomes technological barrier in 3D brain imaging
Scientists at the Swiss Light Source SLS have succeeded in mapping a piece of brain tissue in 3D at unprecedented resolution using X-rays, non-destructively. The breakthrough overcomes a long-standing technological barrier that had limited [...]