The new test could help identify which patients are most likely to benefit from new Alzheimer’s drugs.
A newly developed blood test for Alzheimer’s disease not only helps confirm the presence of the condition but also provides information about how far the disease has progressed, according to research from Washington University School of Medicine in St. Louis and Lund University in Sweden.
While several Alzheimer’s blood tests are already available, including two based on technology licensed from Washington University, those existing tests mainly assist in diagnosing the disease in people showing cognitive symptoms. However, they do not reveal how advanced the symptoms are or the extent of cognitive decline caused by Alzheimer’s dementia. This distinction is important because current treatments for Alzheimer’s are most effective in the early stages. A reliable, accessible method to assess disease progression could help doctors identify which patients are most likely to benefit from treatment and how aggressively they should be treated.
The new test also offers valuable insight into whether a person’s symptoms are due to Alzheimer’s or another underlying condition.
The study was recently published in the journal Nature Medicine.
In the study, the researchers found that levels of a protein called MTBR-tau243 in the blood accurately reflect the amount of toxic accumulation of tau aggregates in the brain and correlate with the severity of Alzheimer’s disease. Analyzing blood levels of MTBR-tau243 from a group of people with cognitive decline, the researchers were able to distinguish between people with early- or later-stage Alzheimer’s disease and separate both groups of Alzheimer’s patients from people whose symptoms were caused by something other than Alzheimer’s disease.
“This blood test clearly identifies Alzheimer’s tau tangles, which is our best biomarker measure of Alzheimer’s symptoms and dementia,” said co-senior author Randall J. Bateman, MD, the Charles F. and Joanne Knight Distinguished Professor of Neurology at WashU Medicine. “In clinical practice right now, we don’t have easy or accessible measures of Alzheimer’s tangles and dementia, and so a tangle blood test like this can provide a much better indication if the symptoms are due to Alzheimer’s and may also help doctors decide which treatments are best for their patients.”
Tracking Alzheimer’s disease progression from blood
Alzheimer’s disease involves a build-up of a protein, called amyloid, into plaques in the brain, followed by the development of tangles of tau protein years later. Cognitive symptoms emerge around the time tau tangles become detectable, and symptoms worsen as the tangles spread. The gold standard for staging Alzheimer’s disease is positron emission tomography (PET) brain scans for amyloid plaques and tau tangles. Amyloid scans yield information about the presymptomatic and early symptomatic stages, while tau scans are useful for tracking later stages of the disease. PET brain scans are highly accurate but expensive, time-consuming, and frequently unavailable outside of major research centers, so they are not widely used.
Bateman leads a team that is developing blood tests for Alzheimer’s disease as a more accessible alternative to brain scans. They have developed two blood tests that correlate closely with the amount of amyloid plaques in the brain. Both are now used by doctors to aid diagnosis. But until now, there has been no blood test that reports on tau levels in the brain.
In a previous study, Bateman and colleagues — including co-first authors Kanta Horie, PhD, a research associate professor of neurology at WashU Medicine, and Gemma Salvadó, PhD, then a postdoctoral researcher at Lund University, and co-senior author Oskar Hansson, MD, PhD, a professor of neurology at Lund University — showed that cerebrospinal fluid levels of MTBR-tau243 correlate closely with tau tangles in the brain. In the current study, the team extended the analysis to blood. A blood sample is easier to collect than cerebrospinal fluid, which is obtained via spinal tap.

The researchers developed a technique to measure MTBR-tau243 levels in people’s blood and compared it to the amount of tau tangles in their brains as measured by brain scans. They piloted the approach on data from two cohorts: volunteers at WashU Medicine’s Charles F. and Joanne Knight Alzheimer Disease Research Center, which included 108 people, and a subset of 55 people from the Swedish BioFINDER-2 cohort. To assess whether the approach was generalizable, they validated it in an independent dataset consisting of the remaining 739 people in the BioFINDER-2 cohort.
The people in the two cohorts represented all but the most severe end of the spectrum of Alzheimer’s disease, from the presymptomatic stage when brain amyloid levels are elevated but people remain cognitively healthy, through early-stage disease with mild cognitive impairments, to late symptomatic disease when patients exhibit full-blown dementia. For comparison, cognitively healthy people with normal amyloid levels, and people with cognitive symptoms due to conditions other than Alzheimer’s disease, were included.
The researchers’ analysis showed that blood MTBR-tau243 levels reflected the amount of tau tangles in the brain with 92% accuracy. MTBR-tau243 levels in the blood were normal in asymptomatic people regardless of amyloid status, meaning that blood MTBR-tau243 levels do not change between healthy people and people in the presymptomatic stage of Alzheimer’s disease with amyloid plaques.
Among people with cognitive symptoms due to Alzheimer’s disease, MTBR-tau243 levels were significantly elevated for people in the mild cognitive impairment phase of Alzheimer’s disease and much higher — up to 200 times — for those in the dementia phase. Those differences translated into clear separation of people in early- and late-stage Alzheimer’s disease. At the same time, MTBR-tau243 levels were normal in people with cognitive symptoms due to diseases other than Alzheimer’s, meaning that the test effectively distinguished Alzheimer’s dementia from other kinds of dementia.
The technology underlying the blood test for tau aggregates has been licensed by WashU to C2N Diagnostics, a WashU startup that developed the blood tests for amyloid. These amyloid tests incorporate measures of another form of tau called p-tau217.
“I believe we will use blood-based p-tau217 to determine whether an individual has Alzheimer’s disease, but MTBR-tau243 will be a highly valuable complement in both clinical settings and research trials,” said Hansson. “When both of these biomarkers are positive, the likelihood that Alzheimer’s is the underlying cause of a person’s cognitive symptoms increases significantly, compared to when only p-tau217 is abnormal. This distinction is crucial for selecting the most appropriate treatment for each patient.”
Blood tests could inform personalized Alzheimer’s treatment
Two Alzheimer’s therapies have been approved by the Food and Drug Administration (FDA) to slow progression of the disease, and both work by lowering amyloid levels in the brain. Horie said the number and variety of available Alzheimer’s medications may soon be expanding, as several experimental drugs that target tau or other aspects of Alzheimer’s disease are in the pipeline. With blood tests to diagnose and stage the disease, doctors would be able to tailor treatments to the patient’s particular disease state.
“We’re about to enter the era of personalized medicine for Alzheimer’s disease,” Horie said. “For early stages with low tau tangles, anti-amyloid therapies could be more efficacious than in late stages. But after the onset of dementia with high tau tangles, anti-tau therapy or one of the many other experimental approaches may be more effective. Once we have a clinically available blood test for staging, plus treatments that work at different stages of the disease, doctors will be able to optimize their treatment plans for the specific needs of each patient.”
Reference: “Plasma MTBR-tau243 biomarker identifies tau tangle pathology in Alzheimer’s disease” by Kanta Horie, Gemma Salvadó, Rama K. Koppisetti, Shorena Janelidze, Nicolas R. Barthélemy, Yingxin He, Chihiro Sato, Brian A. Gordon, Hong Jiang, Tammie L. S. Benzinger, Erik Stomrud, David M. Holtzman, Niklas Mattsson-Carlgren, John C. Morris, Sebastian Palmqvist, Rik Ossenkoppele, Suzanne E. Schindler, Oskar Hansson and Randall J. Bateman, 31 March 2025, Nature Medicine.
DOI: 10.1038/s41591-025-03617-7
This work was supported by the Charles F. and Joanne Knight Alzheimer Disease Research Center; the Tracy Family SILQ Center; the National Institutes of Health (NIH), grant number R01AG070941; the Alzheimer’s Association’s Zenith Award; the Hope Center for Neurological Disorders; and the Department of Neurology at WashU Medicine. The Swedish BioFINDER-2 study was supported by the U.S. National Institute on Aging, grant number R01AG083740, the European Research Council, grant number ADG-101096455; the Alzheimer’s Association, grant numbers ZEN24-1069572 and SG-23-1061717; the GHR Foundation; the Swedish Research Council, grant numbers 2022-00775, 2021-02219, and 2018-02052; ERA PerMed, grant number ERAPERMED2021-184; the Knut and Alice Wallenberg foundation, grant number 2022-0231; the Strategic Research Area MultiPark (Multidisciplinary Research in Parkinson’s disease) at Lund University; the Swedish Alzheimer Foundation, grant numbers AF-980907, AF-994229, and AF-994075; the Swedish Brain Foundation, grant numbers FO2021-0293, FO2023-0163 and FO2022-0204; the Wallenberg AI, Autonomous Systems and Software Program (WASP) and the SciLifeLab and Wallenberg National Program for Data-Driven Life Science (DDLS) joint call for research projects, grant number WASP/DDLS22-066; the Parkinson foundation of Sweden, grant number 1412/22; the Cure Alzheimer’s fund; the Rönström Family Foundation; the Konung Gustaf V:s och Drottning Victorias Frimurarestiftelse; the Skåne University Hospital Foundation, grant number 2020-O000028; the Regionalt Forskningsstöd, grant number 2022-1259; and the Swedish federal government under the ALF agreement, grant numbers 2022-Projekt0080 and 2022-Projekt0107. Gemma Salvadó received funding from the European Union’s Horizon 2020 Research and Innovation Program under Marie Sklodowska-Curie action grant agreement number 101061836; the Alzheimer’s Association, fellowship number AARF-22-972612; the Alzheimerfonden, grant number AF-980942; BrightFocus Foundation, fellowship number A2024007F; Greta och Johan Kocks; and the Strategic Research Area MultiPark (Multidisciplinary Research in Parkinson’s Disease) at Lund University.
News
Scientists May Have Found a Secret Weapon To Stop Pancreatic Cancer Before It Starts
Researchers at Cold Spring Harbor Laboratory have found that blocking the FGFR2 and EGFR genes can stop early-stage pancreatic cancer from progressing, offering a promising path toward prevention. Pancreatic cancer is expected to become [...]
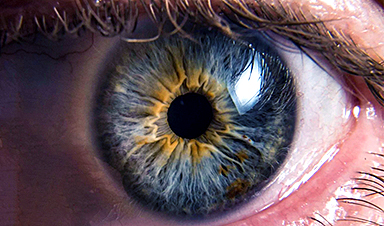
Breakthrough Drug Restores Vision: Researchers Successfully Reverse Retinal Damage
Blocking the PROX1 protein allowed KAIST researchers to regenerate damaged retinas and restore vision in mice. Vision is one of the most important human senses, yet more than 300 million people around the world are at [...]
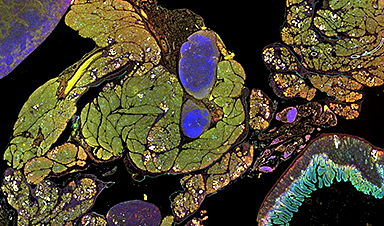
Differentiating cancerous and healthy cells through motion analysis
Researchers from Tokyo Metropolitan University have found that the motion of unlabeled cells can be used to tell whether they are cancerous or healthy. They observed malignant fibrosarcoma cells and [...]
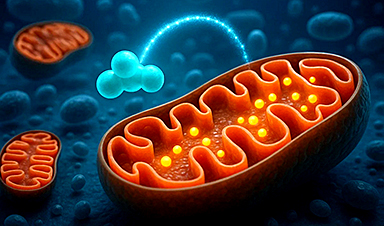
This Tiny Cellular Gate Could Be the Key to Curing Cancer – And Regrowing Hair
After more than five decades of mystery, scientists have finally unveiled the detailed structure and function of a long-theorized molecular machine in our mitochondria — the mitochondrial pyruvate carrier. This microscopic gatekeeper controls how [...]
Unlocking Vision’s Secrets: Researchers Reveal 3D Structure of Key Eye Protein
Researchers have uncovered the 3D structure of RBP3, a key protein in vision, revealing how it transports retinoids and fatty acids and how its dysfunction may lead to retinal diseases. Proteins play a critical [...]
5 Key Facts About Nanoplastics and How They Affect the Human Body
Nanoplastics are typically defined as plastic particles smaller than 1000 nanometers. These particles are increasingly being detected in human tissues: they can bypass biological barriers, accumulate in organs, and may influence health in ways [...]
Measles Is Back: Doctors Warn of Dangerous Surge Across the U.S.
Parents are encouraged to contact their pediatrician if their child has been exposed to measles or is showing symptoms. Pediatric infectious disease experts are emphasizing the critical importance of measles vaccination, as the highly [...]
AI at the Speed of Light: How Silicon Photonics Are Reinventing Hardware
A cutting-edge AI acceleration platform powered by light rather than electricity could revolutionize how AI is trained and deployed. Using photonic integrated circuits made from advanced III-V semiconductors, researchers have developed a system that vastly [...]
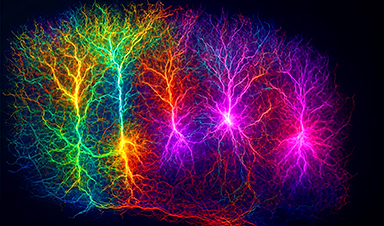
A Grain of Brain, 523 Million Synapses, Most Complicated Neuroscience Experiment Ever Attempted
A team of over 150 scientists has achieved what once seemed impossible: a complete wiring and activity map of a tiny section of a mammalian brain. This feat, part of the MICrONS Project, rivals [...]
The Secret “Radar” Bacteria Use To Outsmart Their Enemies
A chemical radar allows bacteria to sense and eliminate predators. Investigating how microorganisms communicate deepens our understanding of the complex ecological interactions that shape our environment is an area of key focus for the [...]
Psychologists explore ethical issues associated with human-AI relationships
It's becoming increasingly commonplace for people to develop intimate, long-term relationships with artificial intelligence (AI) technologies. At their extreme, people have "married" their AI companions in non-legally binding ceremonies, and at least two people [...]
When You Lose Weight, Where Does It Actually Go?
Most health professionals lack a clear understanding of how body fat is lost, often subscribing to misconceptions like fat converting to energy or muscle. The truth is, fat is actually broken down into carbon [...]
How Everyday Plastics Quietly Turn Into DNA-Damaging Nanoparticles
The same unique structure that makes plastic so versatile also makes it susceptible to breaking down into harmful micro- and nanoscale particles. The world is saturated with trillions of microscopic and nanoscopic plastic particles, some smaller [...]
AI Outperforms Physicians in Real-World Urgent Care Decisions, Study Finds
The study, conducted at the virtual urgent care clinic Cedars-Sinai Connect in LA, compared recommendations given in about 500 visits of adult patients with relatively common symptoms – respiratory, urinary, eye, vaginal and dental. [...]
Challenging the Big Bang: A Multi-Singularity Origin for the Universe
In a study published in the journal Classical and Quantum Gravity, Dr. Richard Lieu, a physics professor at The University of Alabama in Huntsville (UAH), which is a part of The University of Alabama System, suggests that [...]
New drug restores vision by regenerating retinal nerves
Vision is one of the most crucial human senses, yet over 300 million people worldwide are at risk of vision loss due to various retinal diseases. While recent advancements in retinal disease treatments have [...]