Findings supported by the NIH pave the way for the development of genetic testing, clinical trials, and therapies.
Researchers at the National Institutes of Health (NIH) and their collaborators have discovered a gene linked to certain inherited retinal diseases (IRDs). These diseases, which impair the eye’s light-sensitive retina and pose a threat to vision, collectively affect over 2 million people globally. However, each specific disease is rare, making it challenging to gather enough participants for research and clinical trials to develop effective treatments. The findings of the study were published in JAMA Ophthalmology.
In a small study of six unrelated participants, researchers linked the gene UBAP1L to different forms of retinal dystrophies, with issues affecting the macula, the part of the eye used for central vision such as for reading (maculopathy), issues affecting the cone cells that enable color vision (cone dystrophy) or a disorder that also affects the rod cells that enable night vision (cone-rod dystrophy). The patients had symptoms of retinal dystrophy starting in early adulthood, progressing to severe vision loss by late adulthood.

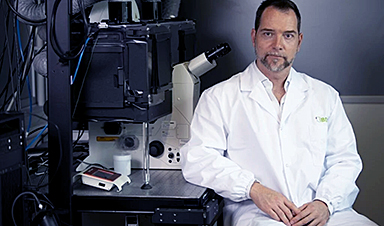
“The patients in this study showed symptoms and features similar to other IRDs, but the cause of their condition was uncertain,” said Bin Guan, Ph.D., chief of the Ophthalmic Genomics Laboratory at NIH’s National Eye Institute (NEI) and a senior author of the report. “Now that we’ve identified the causative gene, we can study how the gene defect causes disease and, hopefully, develop treatment.”
Importance of Genetic Testing in Retinal Dystrophies
Identifying the UBAP1L gene’s involvement adds to the list of more than 280 genes responsible for this heterogeneous disease.
“These findings highlight the importance of providing genetic testing to our patients with retinal dystrophy, and the value of the clinic and lab working together to better understand retinal diseases,” said co-senior author on the paper, Laryssa A. Huryn, M.D., an ophthalmologist at the NEI, part of the National Institutes of Health.
Genetic evaluation of the six patients revealed four variants in the UBAP1L gene, which encodes for a protein that is abundantly expressed in retina cells, including retinal pigment epithelium cells and photoreceptors. More research is needed to understand the UBAP1L gene’s exact function, but scientists were able to determine that the identified variants likely cause the gene to produce protein that lacks function.
Future studies will also be informed by the fact that variants appear to be distinctive to geographic regions. Five of the six families in this study were from South or Southeastern Asia, or Polynesia, regions that have been underrepresented in genetic studies.
Reference: “Biallelic Loss-of-Function Variants in UBAP1L and Nonsyndromic Retinal Dystrophies” by Ehsan Ullah, Siying Lin, Jiaxiong Lu, Chelsea Bender, Andrew R. Webster, Samantha Malka, Savita Madhusudhan, Emma Rees, Denise Williams, Aime R. Agather, Catherine A. Cukras, Robert B. Hufnagel, Rui Chen, Laryssa A. Huryn, Gavin Arno and Bin Guan, 26 September 2024, JAMA Ophthalmology.
DOI: 10.1001/jamaophthalmol.2024.3836
News
Beneficial genetic changes observed in regular blood donors
Researchers at the Francis Crick Institute have identified genetic changes in blood stem cells from frequent blood donors that support the production of new, non-cancerous cells. Understanding the differences in the mutations that accumulate [...]
Shocking Amounts of Microplastics in the Brain – It Could Be Increasing Our Risk of Dementia
The brain has higher concentrations of plastic particles compared to other organs, with increased levels found in dementia patients. In a comprehensive commentary published in Brain Medicine, researchers highlight alarming new evidence of microplastic accumulation [...]
Baffling Scientists for Centuries: New Study Unravels Mystery of Static Electricity
ISTA physicists demonstrate that contact electrification depends on the contact history of materials. For centuries, static electricity has intrigued and perplexed scientists. Now, researchers from the Waitukaitis group at the Institute of Science and [...]
Tumor “Stickiness” – Scientists Develop Potential New Way To Predict Cancer’s Spread
UC San Diego researchers have developed a device that predicts breast cancer aggressiveness by measuring tumor cell adhesion. Weakly adherent cells indicate a higher risk of metastasis, especially in early-stage DCIS. This innovation could [...]
Scientists Just Watched Atoms Move for the First Time Using AI
Scientists have developed a groundbreaking AI-driven technique that reveals the hidden movements of nanoparticles, essential in materials science, pharmaceuticals, and electronics. By integrating artificial intelligence with electron microscopy, researchers can now visualize atomic-level changes that were [...]
Scientists Sound Alarm: “Safe” Antibiotic Has Led to an Almost Untreatable Superbug
A recent study reveals that an antibiotic used for liver disease patients may increase their risk of contracting a dangerous superbug. An international team of researchers has discovered that rifaximin, a commonly prescribed antibiotic [...]
Scientists Discover Natural Compound That Stops Cancer Progression
A discovery led by OHSU was made possible by years of study conducted by University of Portland undergraduates. Scientists have discovered a natural compound that can halt a key process involved in the progression [...]
Scientists Just Discovered an RNA That Repairs DNA Damage – And It’s a Game-Changer
Our DNA is constantly under threat — from cell division errors to external factors like sunlight and smoking. Fortunately, cells have intricate repair mechanisms to counteract this damage. Scientists have uncovered a surprising role played by [...]
What Scientists Just Discovered About COVID-19’s Hidden Death Toll
COVID-19 didn’t just claim lives directly—it reshaped mortality patterns worldwide. A major international study found that life expectancy plummeted across most of the 24 analyzed countries, with additional deaths from cardiovascular disease, substance abuse, and mental [...]
Self-Propelled Nanoparticles Improve Immunotherapy for Non-Invasive Bladder Cancer
A study led by Pohang University of Science and Technology (POSTECH) and the Institute for Bioengineering of Catalonia (IBEC) in South Korea details the creation of urea-powered nanomotors that enhance immunotherapy for bladder cancer. The nanomotors [...]
Scientists Develop New System That Produces Drinking Water From Thin Air
UT Austin researchers have developed a biodegradable, biomass-based hydrogel that efficiently extracts drinkable water from the air, offering a scalable, sustainable solution for water access in off-grid communities, emergency relief, and agriculture. Discarded food [...]
AI Unveils Hidden Nanoparticles – A Breakthrough in Early Disease Detection
Deep Nanometry (DNM) is an innovative technique combining high-speed optical detection with AI-driven noise reduction, allowing researchers to find rare nanoparticles like extracellular vesicles (EVs). Since EVs play a role in disease detection, DNM [...]
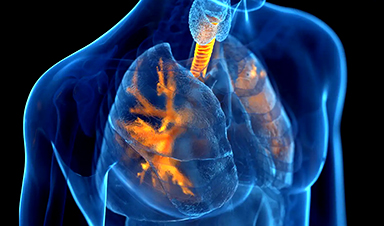
Inhalable nanoparticles could help treat chronic lung disease
Nanoparticles designed to release antibiotics deep inside the lungs reduced inflammation and improved lung function in mice with symptoms of chronic obstructive pulmonary disease By Grace Wade Delivering medication to the lungs with inhalable nanoparticles [...]
New MRI Study Uncovers Hidden Lung Abnormalities in Children With Long COVID
Long COVID is more than just lingering symptoms—it may have a hidden biological basis that standard medical tests fail to detect. A groundbreaking study using advanced MRI technology has uncovered significant lung abnormalities in [...]
AI Struggles with Abstract Thought: Study Reveals GPT-4’s Limits
While GPT-4 performs well in structured reasoning tasks, a new study shows that its ability to adapt to variations is weak—suggesting AI still lacks true abstract understanding and flexibility in decision-making. Artificial Intelligence (AI), [...]
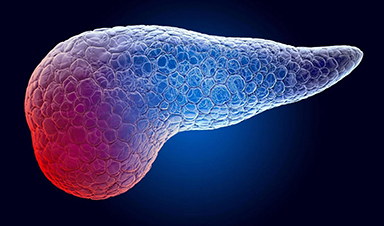
Turning Off Nerve Signals: Scientists Develop Promising New Pancreatic Cancer Treatment
Pancreatic cancer reprograms nerve cells to fuel its growth, but blocking these connections can shrink tumors and boost treatment effectiveness. Pancreatic cancer is closely linked to the nervous system, according to researchers from the [...]