In a recent study published in PLoS Computational Biology, researchers used mathematical modelling to evaluate whether prioritizing older individuals for coronavirus disease 2019 (COVID-19) booster vaccinations consistently leads to optimal public health outcomes across diverse socio-economic settings.
In the early stages of the COVID-19 pandemic, non-pharmaceutical interventions (NPIs) were crucial in reducing transmission and protecting healthcare systems.
The introduction of vaccines, such as those from Pfizer-BioNTech, Oxford-AstraZeneca, and Moderna, significantly altered the pandemic’s trajectory by reducing severe cases and relaxing NPIs.
However, immunity from these vaccines wanes over time, necessitating booster vaccinations, especially with emerging variants.
Further research is needed to refine booster vaccination strategies to address varying population structures and socio-economic contexts globally, ensuring the most effective public health outcomes.
About the study
The study extends a previously published age-structured compartmental model of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) transmission and vaccination.
This deterministic model, governed by ordinary differential equations, divides individuals into compartments based on age, current infection status, and immune status before any infection.
The model includes 16 age groups, with individuals classified as Susceptible, Exposed, Infectious (symptomatic or asymptomatic), or Recovered.
To more accurately represent the time spent in the exposed class, the model employs gamma distributions, which provide a realistic representation of epidemiological periods.
The model also tracks immune status, categorizing individuals into groups such as Vaccinated, Boosted, Partially Waned, Fully Waned, and Unvaccinated, reflecting their infection and vaccination history.
The effectiveness of vaccination is incorporated into the model, accounting for reduced risks of infection, symptoms, hospitalization, and death.
Using this model, the study examines the impacts of six different age-based booster vaccination strategies across eight countries. Strategy 1 prioritizes the oldest individuals first, while Strategy 6 explores vaccinating those with the most contacts to provide indirect protection to the elderly.
Strategies 2-5 test variations of these approaches, generally focusing on prioritizing older individuals for booster vaccination. The analysis assumes limited vaccine availability, with a 10% population coverage baseline and a 90% maximum uptake per age group.
Study results
The population’s age structure varies significantly across countries, with high-income countries generally having a larger proportion of older individuals compared to low-income countries.
This demographic difference influences the distribution of booster vaccines under different vaccination strategies. In the UK, for instance, strategies 1-4 that prioritize older individuals for booster vaccination result in a substantial number of individuals aged 50-74 receiving vaccines. However, the oldest individuals (75+) may not be fully covered due to the limited vaccine supply.
On the other hand, Strategies focused on vaccinating younger individuals, particularly those aged 20-49, who typically have more contacts and, therefore, could potentially contribute to indirect protection of older populations.
However, the age distribution of vaccinated individuals under each strategy varies between countries. For example, in Sierra Leone, where the proportion of older individuals is relatively small, Strategies 1-4 effectively vaccinate almost all older individuals, leading to identical outcomes for these strategies.
This contrasts with the situation in the UK, where a larger elderly population means that not all older individuals can be vaccinated under these strategies due to vaccine constraints.
When considering the impact of these strategies on public health outcomes during a wave of infections caused by a novel SARS-CoV-2 variant, the model projections indicated that Strategy 1 consistently resulted in the fewest deaths across all countries analyzed.
This outcome is particularly evident in high-income countries, where a large proportion of older individuals contribute to a higher projected number of deaths if they are not prioritized for booster vaccination.
In contrast, in countries like Sierra Leone, the small number of older individuals allows nearly all of them to receive booster vaccines under Strategy 1, leading to fewer deaths overall.
The analysis also examined the projected Years of Life Lost (YLL), which accounts for the number of deaths and the ages at which they occur.
While it might be expected that vaccinating younger individuals could reduce YLL, the model consistently showed that Strategy 1, which prioritizes the oldest individuals, was optimal in minimizing YLL. This is due to the higher risk of severe outcomes and mortality associated with SARS-CoV-2 infection in older populations.
Sensitivity analyses further supported these findings, showing that Strategy 1 led to fewer deaths and YLL under various assumptions, including different levels of vaccine availability, uptake rates, and timing of booster administration.
Even when the outbreak began 150 days after booster vaccines were administered, resulting in some immunity waning, Strategy 1 remained the most effective approach in reducing deaths and YLL.
Conclusions
To summarize, future SARS-CoV-2 transmission will be influenced by novel variants, booster vaccinations, and immunity dynamics. Unlike the pandemic’s early stages, many individuals globally are now infected or vaccinated, impacting immunity and transmission.
In this evolving scenario, it is essential to reassess the effectiveness of past interventions and explore new strategies.
This study evaluated different age-based booster vaccination strategies and found that prioritizing older individuals consistently leads to better public health outcomes, regardless of varying population structures.
- Bouros I, Hill EM, Keeling MJ, et al. (2024) Prioritizing older individuals for COVID-19 booster vaccination leads to optimal public health outcomes in a range of socio-economic settings. PLoS Comput Biol. doi:https://doi.org/10.1371/journal. pcbi.1012309. https://journals.plos.org/ploscompbiol/article?
News
Studies detail high rates of long COVID among healthcare, dental workers
Researchers have estimated approximately 8% of Americas have ever experienced long COVID, or lasting symptoms, following an acute COVID-19 infection. Now two recent international studies suggest that the percentage is much higher among healthcare workers [...]
Melting Arctic Ice May Unleash Ancient Deadly Diseases, Scientists Warn
Melting Arctic ice increases human and animal interactions, raising the risk of infectious disease spread. Researchers urge early intervention and surveillance. Climate change is opening new pathways for the spread of infectious diseases such [...]
Scientists May Have Found a Secret Weapon To Stop Pancreatic Cancer Before It Starts
Researchers at Cold Spring Harbor Laboratory have found that blocking the FGFR2 and EGFR genes can stop early-stage pancreatic cancer from progressing, offering a promising path toward prevention. Pancreatic cancer is expected to become [...]
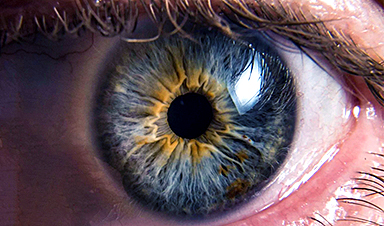
Breakthrough Drug Restores Vision: Researchers Successfully Reverse Retinal Damage
Blocking the PROX1 protein allowed KAIST researchers to regenerate damaged retinas and restore vision in mice. Vision is one of the most important human senses, yet more than 300 million people around the world are at [...]
Differentiating cancerous and healthy cells through motion analysis
Researchers from Tokyo Metropolitan University have found that the motion of unlabeled cells can be used to tell whether they are cancerous or healthy. They observed malignant fibrosarcoma cells and [...]
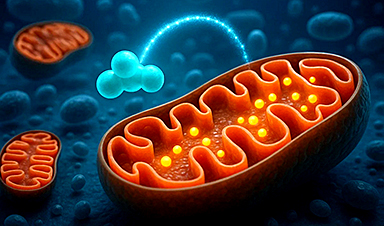
This Tiny Cellular Gate Could Be the Key to Curing Cancer – And Regrowing Hair
After more than five decades of mystery, scientists have finally unveiled the detailed structure and function of a long-theorized molecular machine in our mitochondria — the mitochondrial pyruvate carrier. This microscopic gatekeeper controls how [...]
Unlocking Vision’s Secrets: Researchers Reveal 3D Structure of Key Eye Protein
Researchers have uncovered the 3D structure of RBP3, a key protein in vision, revealing how it transports retinoids and fatty acids and how its dysfunction may lead to retinal diseases. Proteins play a critical [...]
5 Key Facts About Nanoplastics and How They Affect the Human Body
Nanoplastics are typically defined as plastic particles smaller than 1000 nanometers. These particles are increasingly being detected in human tissues: they can bypass biological barriers, accumulate in organs, and may influence health in ways [...]
Measles Is Back: Doctors Warn of Dangerous Surge Across the U.S.
Parents are encouraged to contact their pediatrician if their child has been exposed to measles or is showing symptoms. Pediatric infectious disease experts are emphasizing the critical importance of measles vaccination, as the highly [...]
AI at the Speed of Light: How Silicon Photonics Are Reinventing Hardware
A cutting-edge AI acceleration platform powered by light rather than electricity could revolutionize how AI is trained and deployed. Using photonic integrated circuits made from advanced III-V semiconductors, researchers have developed a system that vastly [...]
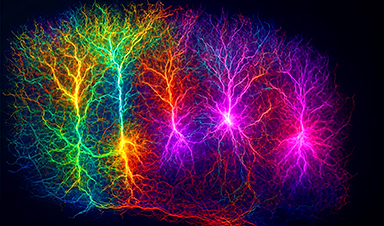
A Grain of Brain, 523 Million Synapses, Most Complicated Neuroscience Experiment Ever Attempted
A team of over 150 scientists has achieved what once seemed impossible: a complete wiring and activity map of a tiny section of a mammalian brain. This feat, part of the MICrONS Project, rivals [...]
The Secret “Radar” Bacteria Use To Outsmart Their Enemies
A chemical radar allows bacteria to sense and eliminate predators. Investigating how microorganisms communicate deepens our understanding of the complex ecological interactions that shape our environment is an area of key focus for the [...]
Psychologists explore ethical issues associated with human-AI relationships
It's becoming increasingly commonplace for people to develop intimate, long-term relationships with artificial intelligence (AI) technologies. At their extreme, people have "married" their AI companions in non-legally binding ceremonies, and at least two people [...]
When You Lose Weight, Where Does It Actually Go?
Most health professionals lack a clear understanding of how body fat is lost, often subscribing to misconceptions like fat converting to energy or muscle. The truth is, fat is actually broken down into carbon [...]
How Everyday Plastics Quietly Turn Into DNA-Damaging Nanoparticles
The same unique structure that makes plastic so versatile also makes it susceptible to breaking down into harmful micro- and nanoscale particles. The world is saturated with trillions of microscopic and nanoscopic plastic particles, some smaller [...]
AI Outperforms Physicians in Real-World Urgent Care Decisions, Study Finds
The study, conducted at the virtual urgent care clinic Cedars-Sinai Connect in LA, compared recommendations given in about 500 visits of adult patients with relatively common symptoms – respiratory, urinary, eye, vaginal and dental. [...]