Researchers have pinpointed specific variants in a gene that significantly raise the likelihood of developing various cancer types. This discovery has the potential to enhance early detection and facilitate personalized treatments for diverse populations.
Scientists have identified over 5,000 genetic variants that help certain cancers thrive, as well as a potential therapeutic target that could treat or possibly prevent these cancers from developing.
Researchers from the Wellcome Sanger Institute, and their collaborators at The Institute of Cancer Research, London, and the University of Cambridge assessed the health impact of all possible genetic changes in the 'tumour protection' gene, BAP1. They found around a fifth of these possible changes were pathogenic, significantly increasing the risk of developing cancers of the eye, lung lining, brain, skin, and kidney.
The findings, published in Nature Genetics, are freely available so that they can be immediately used by doctors to help diagnose patients and choose the most effective therapies for them. Importantly, as all possible variants were assessed, the findings benefit individuals from diverse ethnic backgrounds, who have historically been underrepresented in genetics research.
Potential for New Cancer Therapies
The team also uncovered a link between certain disruptive BAP1 variants and higher levels of IGF-1, a hormone and growth factor. This discovery opens the door to developing new drugs that could inhibit these harmful effects, potentially slowing down or preventing the progression of certain cancers.
The BAP1 protein acts as a powerful tumor suppressor in the body, protecting against cancers of the eye, lung lining, brain, skin, and kidney. Inherited variants that disrupt the protein can increase a person's lifetime risk of developing these cancers by up to 50 per cent, typically occurring around middle age.
Detecting these variants early through genetic screening can guide preventative measures, greatly enhance treatment effectiveness, and improve the quality of life for individuals affected. However, until now, there has been limited understanding of which specific genetic changes in BAP1 to look out for, especially for rare variants that cause it to malfunction and fuel cancer growth.
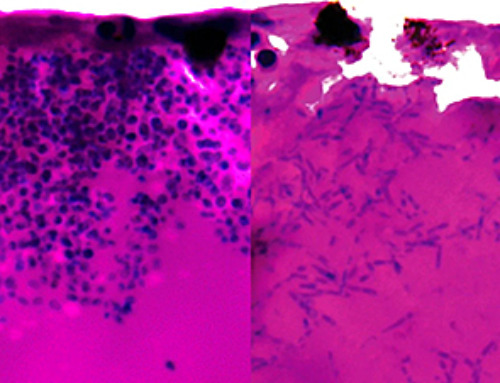
Researchers from the Sanger Institute, and their collaborators at The Institute of Cancer Research and the University of Cambridge tested all 18,108 possible DNA changes in the BAP1 gene by artificially altering the genetic code of human cells grown in a dish, in a process known as 'saturation genome editing'. They identified that 5,665 of these changes were harmful and disrupted the protein's protective effects. Analysis of UK Biobank data confirmed that individuals carrying these harmful BAP1 variants are over ten percent more likely to be diagnosed with cancer than the general population.
Link Between BAP1 Variants and IGF-1 Levels
The team also discovered that people with harmful BAP1 variants have elevated levels of IGF-1 in their blood, a hormone linked to both cancer growth and brain development. Even individuals without cancer showed these elevated levels, suggesting that IGF-1 could be a target for new treatments to slow down or prevent certain cancers. Further analysis revealed harmful BAP1 variants and higher IGF-1 levels were linked to worse outcomes in uveal melanoma patients, highlighting the potential for IGF-1 inhibitors in cancer therapy.
Notably, the technique profiles all possible BAP1 variants from diverse populations, not only those prevalent in European clinical records, helping to address the underrepresentation of non-European populations in genetic studies.
Dr Andrew Waters, first author of the study at the Wellcome Sanger Institute, said: "Previous approaches for studying how variants affect function in genes have been on a very small scale, or exclude important contexts that may contribute to how they behave. Our approach provides a true picture of gene behavior, enabling larger and more complex studies of genetic variation. This opens up new possibilities for understanding how these changes drive disease."
Professor Clare Turnbull, clinical lead of the study, Professor of Translational Cancer Genetics at The Institute of Cancer Research, London, and Consultant in Clinical Cancer Genetics at The Royal Marsden NHS Foundation, said: "This research could mean more accurate interpretation of genetic tests, earlier diagnoses and improved outcomes for patients and their families."
Dr David Adams, senior author of the study at the Wellcome Sanger Institute, said: "We want to ensure that life-saving genetic insights are accessible and relevant to all people, regardless of their ancestry. Our aim is to apply this technique to a wider range of genes, potentially covering the entire human genome in the next decade with the Atlas of Variant Effects."
Reference: "Saturation genome editing of BAP1 functionally classifies somatic and germline variants" by Andrew J. Waters, Timothy Brendler-Spaeth, Danielle Smith, Victoria Offord, Hong Kee Tan, Yajie Zhao, Sofia Obolenski, Maartje Nielsen, Remco van Doorn, Jo-Ellen Murphy, Prashant Gupta, Charlie F. Rowlands, Helen Hanson, Erwan Delage, Mark Thomas, Elizabeth J. Radford, Sebastian S. Gerety, Clare Turnbull, John R. B. Perry, Matthew E. Hurles and David J. Adams, 5 July 2024, Nature Genetics.
DOI: 10.1038/s41588-024-01799-3
The study was funded by the Wellcome Trust and Cancer Research UK.
News
AI Helped Scientists Stop a Virus With One Tiny Change
Using AI, researchers identified one tiny molecular interaction that viruses need to infect cells. Disrupting it stopped the virus before infection could begin. Washington State University scientists have uncovered a method to interfere with a key [...]
Deadly Hospital Fungus May Finally Have a Weakness
A deadly, drug-resistant hospital fungus may finally have a weakness—and scientists think they’ve found it. Researchers have identified a genetic process that could open the door to new treatments for a dangerous fungal infection [...]
Fever-Proof Bird Flu Variant Could Fuel the Next Pandemic
Bird flu viruses present a significant risk to humans because they can continue replicating at temperatures higher than a typical fever. Fever is one of the body’s main tools for slowing or stopping viral [...]
What could the future of nanoscience look like?
Society has a lot to thank for nanoscience. From improved health monitoring to reducing the size of electronics, scientists’ ability to delve deeper and better understand chemistry at the nanoscale has opened up numerous [...]
Scientists Melt Cancer’s Hidden “Power Hubs” and Stop Tumor Growth
Researchers discovered that in a rare kidney cancer, RNA builds droplet-like hubs that act as growth control centers inside tumor cells. By engineering a molecular switch to dissolve these hubs, they were able to halt cancer [...]
Platelet-inspired nanoparticles could improve treatment of inflammatory diseases
Scientists have developed platelet-inspired nanoparticles that deliver anti-inflammatory drugs directly to brain-computer interface implants, doubling their effectiveness. Scientists have found a way to improve the performance of brain-computer interface (BCI) electrodes by delivering anti-inflammatory drugs directly [...]
After 150 years, a new chapter in cancer therapy is finally beginning
For decades, researchers have been looking for ways to destroy cancer cells in a targeted manner without further weakening the body. But for many patients whose immune system is severely impaired by chemotherapy or radiation, [...]
Older chemical libraries show promise for fighting resistant strains of COVID-19 virus
SARS‑CoV‑2, the virus that causes COVID-19, continues to mutate, with some newer strains becoming less responsive to current antiviral treatments like Paxlovid. Now, University of California San Diego scientists and an international team of [...]
Lower doses of immunotherapy for skin cancer give better results, study suggests
According to a new study, lower doses of approved immunotherapy for malignant melanoma can give better results against tumors, while reducing side effects. This is reported by researchers at Karolinska Institutet in the Journal of the National [...]
Researchers highlight five pathways through which microplastics can harm the brain
Microplastics could be fueling neurodegenerative diseases like Alzheimer's and Parkinson's, with a new study highlighting five ways microplastics can trigger inflammation and damage in the brain. More than 57 million people live with dementia, [...]
Tiny Metal Nanodots Obliterate Cancer Cells While Largely Sparing Healthy Tissue
Scientists have developed tiny metal-oxide particles that push cancer cells past their stress limits while sparing healthy tissue. An international team led by RMIT University has developed tiny particles called nanodots, crafted from a metallic compound, [...]
Gold Nanoclusters Could Supercharge Quantum Computers
Researchers found that gold “super atoms” can behave like the atoms in top-tier quantum systems—only far easier to scale. These tiny clusters can be customized at the molecular level, offering a powerful, tunable foundation [...]
A single shot of HPV vaccine may be enough to fight cervical cancer, study finds
WASHINGTON -- A single HPV vaccination appears just as effective as two doses at preventing the viral infection that causes cervical cancer, researchers reported Wednesday. HPV, or human papillomavirus, is very common and spread [...]
New technique overcomes technological barrier in 3D brain imaging
Scientists at the Swiss Light Source SLS have succeeded in mapping a piece of brain tissue in 3D at unprecedented resolution using X-rays, non-destructively. The breakthrough overcomes a long-standing technological barrier that had limited [...]
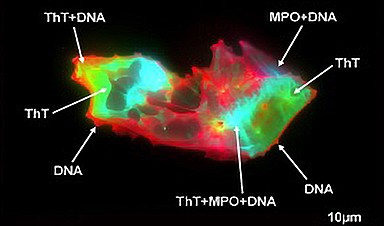
Scientists Uncover Hidden Blood Pattern in Long COVID
Researchers found persistent microclot and NET structures in Long COVID blood that may explain long-lasting symptoms. Researchers examining Long COVID have identified a structural connection between circulating microclots and neutrophil extracellular traps (NETs). The [...]
This Cellular Trick Helps Cancer Spread, but Could Also Stop It
Groups of normal cbiells can sense far into their surroundings, helping explain cancer cell migration. Understanding this ability could lead to new ways to limit tumor spread. The tale of the princess and the [...]