UCLA researchers have identified placental growth factor (PlGF) as a potential blood biomarker for early detection of cognitive impairment and dementia.
High PlGF levels correlate with increased vascular permeability, suggesting its role in the development of cerebral small vessel disease. This finding could enable earlier identification and intervention for at-risk individuals compared to current MRI-based diagnostics.
Vascular Changes and Dementia
Researchers and clinicians typically use MRI scans to track brain blood vessel changes linked to cognitive impairment and dementia. These scans detect “downstream” biological markers — signs that appear later in the disease process. However, a multicenter study led by UCLA researchers suggests that a simple blood test could spot earlier changes, potentially identifying at-risk patients sooner and at a lower cost.
“We studied a protein in the blood that is critical in the formation of blood vessels but that also appears to play a role in vascular permeability associated with cognitive decline,” explained Jason Hinman, MD, PhD, a vascular neurologist at UCLA Health, Interim Co-Director of the Mary S. Easton Center for Alzheimer’s Research and Care at David Geffen School of Medicine at UCLA and senior author of an article in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
“Evaluating data from a large group of patients with a range of vascular risk profiles and cognition ranging from unimpaired to mild dementia, we found that plasma levels of this protein, placental growth factor (PlGF), could potentially be used as a biomarker to screen for and monitor cognitive impairment and dementia.”
Cerebral Small Vessel Disease and Biomarkers
Dysfunctional cells lining blood vessels in the brain are increasingly recognized as a key driver of processes leading to cerebral small vessel disease (CSVD), a major contributor to cognitive decline and dementia. The leaky vessels are believed to allow fluid and inflammatory molecules to seep into brain tissue. CSVD is typically diagnosed through costly brain MRI, where areas of vascular-mediated brain injury appear as bright spots on clinical MRI sequences – called white matter hyperintensities, or WMH. WMH and other structural changes are late markers of vascular brain injury.
Potential of PlGF as a Biomarker
The researchers studied possible associations involving several factors: plasma levels of PlGF, a highly sensitive research MRI measure of fluid accumulation in the brain called white matter free water (FW), white matter hyperintensities, and patients’ scores on cognitive assessments. Results were consistent with models suggesting that elevated PlGF increases vascular permeability, leading to accumulation of fluid in the brain’s white matter, development of white matter hyperintensities, and subsequent cognitive impairment.
“As a biomarker for cerebral small vessel disease and the vascular contributions to cognitive impairment and dementia (VCID), PlGF could be used as a cost-effective screening tool for identifying patients at risk for vascular brain injury before the insidious onset of cognitive decline,” said first author Kyle Kern, MD, a vascular neurologist at UCLA Health and researcher at David Geffen School of Medicine at UCLA. “As a simple blood test, such a tool would be valuable not only for patients and clinicians, but also for researchers identifying patients for clinical trials,” he said.
Study Design and Future Directions
The study was conducted by researchers involved in MarkVCID, a multisite consortium established to validate candidate biomarkers for CSVD through recruitment of participants from diverse racial and ethnic backgrounds, with a range of vascular risk factors, and across the spectrum of cognitive impairment. Participants were 55 or older and had undergone brain MRI and blood tests for PlGF levels.
The authors said that while the study’s multicenter design and large, diverse sample support the use of PlGF as a biomarker, additional longitudinal studies are needed to reach conclusions about causation and timing in the relationships among PlGF, FW, WMH, and cognition. Ideally, PlGF could be used to screen younger populations for whom currently available treatments and lifestyle modifications may prevent or reverse the deleterious effects of vascular injury before the onset of cognitive dysfunction. The research group is recruiting patients for future studies.
Reference: “White matter free water mediates the associations between placental growth factor, white matter hyperintensities, and cognitive status” 18 December 2024, Alzheimer’s & Dementia.
DOI: 10.1002/alz.14408
Funding: National Institutes of Health, Grant/Award Numbers: U24NS100591, UH2NS100599, UH2/UH3NS100605, UH2NS100588, UH2NS100608, UH2NS100606, UH2NS100598, UH2NS100614, UF1NS125513, the BrightFocus Foundation.
News
Measles Is Back: Doctors Warn of Dangerous Surge Across the U.S.
Parents are encouraged to contact their pediatrician if their child has been exposed to measles or is showing symptoms. Pediatric infectious disease experts are emphasizing the critical importance of measles vaccination, as the highly [...]
AI at the Speed of Light: How Silicon Photonics Are Reinventing Hardware
A cutting-edge AI acceleration platform powered by light rather than electricity could revolutionize how AI is trained and deployed. Using photonic integrated circuits made from advanced III-V semiconductors, researchers have developed a system that vastly [...]
A Grain of Brain, 523 Million Synapses, Most Complicated Neuroscience Experiment Ever Attempted
A team of over 150 scientists has achieved what once seemed impossible: a complete wiring and activity map of a tiny section of a mammalian brain. This feat, part of the MICrONS Project, rivals [...]
The Secret “Radar” Bacteria Use To Outsmart Their Enemies
A chemical radar allows bacteria to sense and eliminate predators. Investigating how microorganisms communicate deepens our understanding of the complex ecological interactions that shape our environment is an area of key focus for the [...]
Psychologists explore ethical issues associated with human-AI relationships
It's becoming increasingly commonplace for people to develop intimate, long-term relationships with artificial intelligence (AI) technologies. At their extreme, people have "married" their AI companions in non-legally binding ceremonies, and at least two people [...]
When You Lose Weight, Where Does It Actually Go?
Most health professionals lack a clear understanding of how body fat is lost, often subscribing to misconceptions like fat converting to energy or muscle. The truth is, fat is actually broken down into carbon [...]
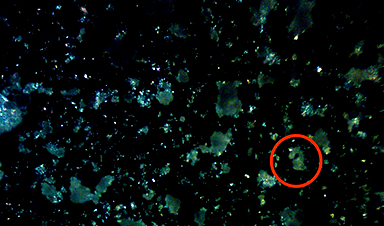
How Everyday Plastics Quietly Turn Into DNA-Damaging Nanoparticles
The same unique structure that makes plastic so versatile also makes it susceptible to breaking down into harmful micro- and nanoscale particles. The world is saturated with trillions of microscopic and nanoscopic plastic particles, some smaller [...]
AI Outperforms Physicians in Real-World Urgent Care Decisions, Study Finds
The study, conducted at the virtual urgent care clinic Cedars-Sinai Connect in LA, compared recommendations given in about 500 visits of adult patients with relatively common symptoms – respiratory, urinary, eye, vaginal and dental. [...]
Challenging the Big Bang: A Multi-Singularity Origin for the Universe
In a study published in the journal Classical and Quantum Gravity, Dr. Richard Lieu, a physics professor at The University of Alabama in Huntsville (UAH), which is a part of The University of Alabama System, suggests that [...]
New drug restores vision by regenerating retinal nerves
Vision is one of the most crucial human senses, yet over 300 million people worldwide are at risk of vision loss due to various retinal diseases. While recent advancements in retinal disease treatments have [...]
Shingles vaccine cuts dementia risk by 20%, new study shows
A shingles shot may do more than prevent rash — it could help shield the aging brain from dementia, according to a landmark study using real-world data from the UK. A routine vaccine could [...]
AI Predicts Sudden Cardiac Arrest Days Before It Strikes
AI can now predict deadly heart arrhythmias up to two weeks in advance, potentially transforming cardiac care. Artificial intelligence could play a key role in preventing many cases of sudden cardiac death, according to [...]
NanoApps Medical is a Top 20 Feedspot Nanotech Blog
There is an ocean of Nanotechnology news published every day. Feedspot saves us a lot of time and we recommend it. We have been using it since 2018. Feedspot is a freemium online RSS [...]
This Startup Says It Can Clean Your Blood of Microplastics
This is a non-exhaustive list of places microplastics have been found: Mount Everest, the Mariana Trench, Antarctic snow, clouds, plankton, turtles, whales, cattle, birds, tap water, beer, salt, human placentas, semen, breast milk, feces, testicles, [...]
New Blood Test Detects Alzheimer’s and Tracks Its Progression With 92% Accuracy
The new test could help identify which patients are most likely to benefit from new Alzheimer’s drugs. A newly developed blood test for Alzheimer’s disease not only helps confirm the presence of the condition but also [...]
The CDC buried a measles forecast that stressed the need for vaccinations
This story was originally published on ProPublica, a nonprofit newsroom that investigates abuses of power. Sign up to receive our biggest stories as soon as they’re published. ProPublica — Leaders at the Centers for Disease Control and Prevention [...]