Stanford Medicine researchers have developed a new method for influenza vaccination that encourages a robust immune response to all four common flu subtypes, potentially increasing the vaccine’s efficacy.
In laboratory tests using human tonsil organoids, the modified vaccine showed promising results in combating both seasonal and bird flu strains. The approach involves a combined antigen methodology that might also protect against emerging flu variants with pandemic potential.
Innovative Flu Vaccine Development
Stanford Medicine scientists have developed a method to make seasonal flu vaccines more effective and potentially protect against emerging flu strains with pandemic potential. Their approach, demonstrated using cultured human tonsil tissue, was published in the journal Science on December 19.
Flu season is a serious health concern. Each year, influenza kills hundreds of thousands of people and hospitalizes millions worldwide. The seasonal flu vaccine helps by priming the immune system for a faster and stronger response. A critical part of this defense involves antibodies — specialized proteins that bind to the flu virus like puzzle pieces. When antibodies attach correctly, they block the virus from entering and multiplying in our cells.
Understanding Vaccine Antigens
Any classical vaccine displays, in a non-threatening way, one or more of a pathogen’s immune-system-arousing biochemical features, or antigens, to various cells of the immune system whose job is to carefully note and memorize particular antigens belonging to the pathogen of interest — the one the vaccine targets. When the real thing comes along, that memory will kick in and rouse those otherwise dormant immune cells to jump up, pump up, and punch out the pest’s lights — preferably before it can invade any cells.
Vaccine Design and Effectiveness
The influenza virus is studded with molecular hooks that it uses to latch on to vulnerable cells in our airways and lungs. This hook-like molecule, called hemagglutinin, is the principal antigen in the influenza vaccine.
The standard flu vaccine contains a mix of four versions of hemagglutinin — one for each of four commonly circulating influenza subtypes. The goal is to protect us from whichever of those subtypes eventually slips through our nostrils and takes up residence in our airways.
The vaccine’s efficacy isn’t as high as it could be, though. In recent years its effectiveness has ranged between about 20% and 80%, said Mark Davis, PhD, professor of microbiology and immunology and the Burt and Marion Avery Family Professor of Immunology.
That’s largely because many vaccinated people fail to develop enough antibodies to one or more of the subtypes represented in the vaccine, said Davis, the study’s senior author. The lead author is Vamsee Mallajosyula, PhD, a basic science research associate in Davis’ lab.
Strangely, most of us develop a robust antibody response to only one of them, Davis said. But he and his colleagues have figured out why that happens and have found a way to force our immune systems to mount a strong antibody response to all four subtypes. That could make a huge difference in the vaccine’s ability to keep us from suffering even mild consequences from influenza infections, let alone more severe ones.
Exploring Immune Response Mechanisms
It’s widely believed that individuals’ immune responses are partially due to what immunologists refer to, tongue in cheek, as “original antigenic sin,” Davis said. “The idea is that our first exposure to a flu infection predisposes us to mount a response to whatever subtype that infecting virus belonged to. Subsequent influenza exposures, regardless of which viral subtype is now assaulting us, will trigger a preferential or even exclusive response to that first subtype.” It’s been thought that we’re marked for life, immunologically speaking, by that initial encounter regardless of which subtype is bugging us now.
But that’s not true. An analysis conducted by Mallajosyula showed that it’s mostly our genes, not our first exposure, that push our immune systems to mount an antibody response to one or another of a flu shot’s four subtypes. Mallajosyula found this uneven immune response to different influenza subtypes (what immunologists call “subtype bias”) in most people, including 77% of identical twins — and 73% of newborns, who’ve had no previous exposure to the flu virus or the vaccine for it.
Davis’ group has found a way to trick our immune systems into paying attention to all four subtypes represented in the vaccine. Here’s how it works.
Overcoming Subtype Bias in Vaccines
B cells — the immune cells that serve as our body’s antibody factories — are ultrapicky about exactly which antibodies they make. An individual B cell will produce only a single species of antibody fitting a mere one or very few antigenic shapes. That B cell is just as picky about what antigen it will pay attention to: that is, precisely the antigen the B cell’s antibodies will stick to. When this antigen comes along, the B cell recognizes it and gobbles it up.
That’s step one.
Next, the B cell chops the antigen up into tiny strips called peptides, which it displays on its surface for inspection by roving immune cells called helper T cells, whose follow-on stimulatory services are critical for turning antigen-displaying B cells into antibody-spewing B cells.
Helper T cells are just as finicky as B cells. A helper T cell will sprinkle its stardust only on B cells displaying antigen-derived peptides that particular T cell is designed to respond to — and even then, only when that peptide is gripped by one of the matching molecular jewel cases that B cells produce in myriad varieties.
But different peptides require different jewel cases. And depending on their luck in the genetic draw, people’s repertoires of those specialized jewel cases vary from one person to the next, leaving many of us with plenty of the jewel cases that match peptides from one influenza-subtype hemagglutinin but far fewer of those that match another flu subtype’s peptides.
In the standard flu vaccine formulation, the four antigens corresponding to the four common subtypes are delivered as separate particles in a mix. To overcome subtype bias, Davis, Mallajosyula, and their colleagues stitched all four antigens together. They designed a vaccine in which the four hemagglutinin varieties are chemically conjoined on a molecular matrix scaffolding. That way, any B cell that recognizes and begins ingesting one or another of the vaccine’s four hemagglutinin types ends up wolfing down the entire matrix and displaying bits of all four antigens on its surface, persuading the immune system to react to all of them despite its predisposition not to.
Forcing B cells to “eat their broccoli” — internalize all four hemagglutinin subtypes instead of just the one that tastes best — effectively multiplies the number of B cells displaying hemagglutinin-derived peptides from every subtype on their surfaces, albeit still in a ratio skewed by the B cells’ uneven inventories of jewel-case molecules.
This, in turn, makes helper T cells much more likely to stumble on a sample from the antigen they love to hate. They fire up, start multiplying feverishly, branch out in pursuit of any B cells displaying that antigen and spur antibody production in them. These selected B cells also proliferate, culminating in bulk production of antibodies that are likely to stop the influenza virus — whatever its subtype — in its tracks.
Testing the New Vaccine
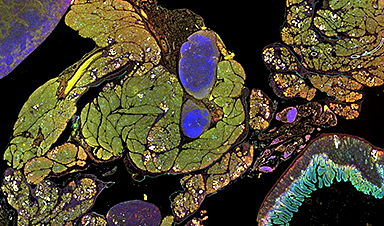
Davis, Mallajosyula and their colleagues tested their four-antigen vaccine construct by putting it into cultures containing human tonsil organoids — living lymph tissue originating from tonsils extracted from tonsillitis patients and then disaggregated. In a laboratory dish, the tissue spontaneously reconstitutes itself into small tonsil spheres, each a “mini-me” that acts just like a lymph node — the ideal environment for antibody manufacturing.
Sure enough, B cells in these organoids that recognized any of the four conjoined hemagglutinin molecules swallowed the whole matrix and, potentially, displayed bits of all four subtypes, thus recruiting far more helper T cells to kick-start their activation. The result was solid antibody responses to all four influenza strains.
Addressing Pandemic Potential
There is considerable concern about a viral strain that could cause the next devastating pandemic: namely avian or “bird flu,” which recently has been detected in wastewater and milk in California, Texas, and other parts of the United States. While this type of flu is not yet able to be transmitted easily between human beings, it could mutate to gain this ability and thus is considered a major risk-in-waiting.
The scientists further showed that they could substantially boost the antibody response to bird flu by vaccinating tonsil organoids with a five-antigen construct connecting the four seasonal antigens along with the bird-flu hemagglutinin, as opposed to getting a tepid response when vaccinating with just the bird-flu hemagglutinin or combining it with the four seasonal antigens on different constructs.
“Overcoming subtype bias this way can lead to a much more effective influenza vaccine, extending even to strains responsible for bird flu,” Davis said. “The bird flu could very likely generate our next viral pandemic.”
For more on this research, see Unlocking the Genetic Code to Supercharge Flu Vaccines.
Reference: “Coupling antigens from multiple subtypes of influenza can broaden antibody and T cell responses” by Vamsee Mallajosyula, Saborni Chakraborty, Elsa Sola, Ryan Furuichi Fong, Vishnu Shankar, Fei Gao, Allison R. Burrell, Neha Gupta, Lisa E. Wagar, Paul S. Mischel, Robson Capasso, Mary A. Staat, Yueh-Hsiu Chien, Cornelia L. Dekker, Taia T. Wang and Mark M. Davis, 19 December 2024, Science.
DOI: 10.1126/science.adi2396
Researchers from the University of Cincinnati College of Medicine contributed to the work.
Davis and Mallajosyula are co-inventors on a patent Stanford’s Office of Technology Licensing has filed for intellectual property related to their coupled-antigen methodology.
The study was funded by National Institutes of Health (grants 5U19AI090019, 5U19AI057229, 5U01AI144673, 75N93019C00051 and U01AI144616) and the Howard Hughes Medical Institute.
News
How the FDA opens the door to risky chemicals in America’s food supply
Lining the shelves of American supermarkets are food products with chemicals linked to health concerns. To a great extent, the FDA allows food companies to determine for themselves whether their ingredients and additives are [...]
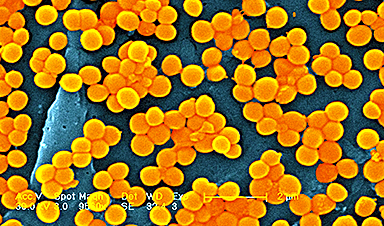
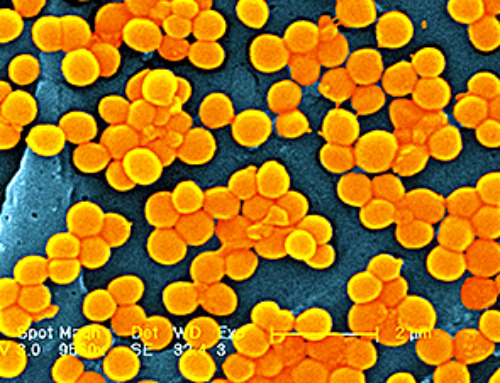
Superbug crisis could get worse, killing nearly 40 million people by 2050
The number of lives lost around the world due to infections that are resistant to the medications intended to treat them could increase nearly 70% by 2050, a new study projects, further showing the [...]
How Can Nanomaterials Be Programmed for Different Applications?
Nanomaterials are no longer just small—they are becoming smart. Across fields like medicine, electronics, energy, and materials science, researchers are now programming nanomaterials to behave in intentional, responsive ways. These advanced materials are designed [...]
Microplastics Are Invading Our Arteries, and It Could Be Increasing Your Risk of Stroke
Higher levels of micronanoplastics were found in carotid artery plaque, especially in people with stroke symptoms, suggesting a potential new risk factor. People with plaque buildup in the arteries of their neck have been [...]
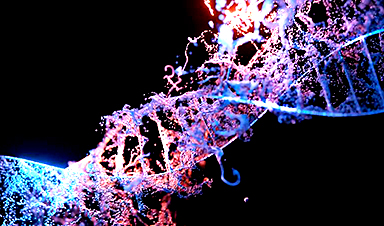
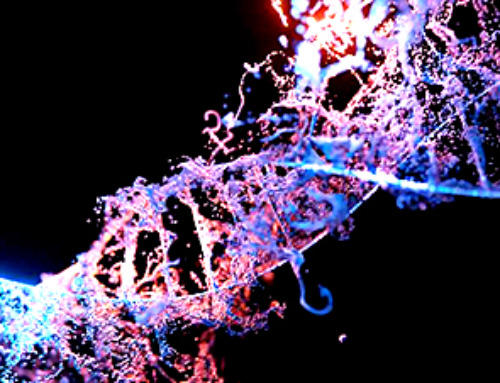
Gene-editing therapy shows early success in fighting advanced gastrointestinal cancers
Researchers at the University of Minnesota have completed a first-in-human clinical trial testing a CRISPR/Cas9 gene-editing technique to help the immune system fight advanced gastrointestinal (GI) cancers. The results, recently published in The Lancet Oncology, show encouraging [...]
Engineered extracellular vesicles facilitate delivery of advanced medicines
Graphic abstract of the development of VEDIC and VFIC systems for high efficiency intracellular protein delivery in vitro and in vivo. Credit: Nature Communications (2025). DOI: 10.1038/s41467-025-59377-y. https://www.nature.com/articles/s41467-025-59377-y Researchers at Karolinska Institutet have developed a technique [...]
Brain-computer interface allows paralyzed users to customize their sense of touch
University of Pittsburgh School of Medicine scientists are one step closer to developing a brain-computer interface, or BCI, that allows people with tetraplegia to restore their lost sense of touch. While exploring a digitally [...]
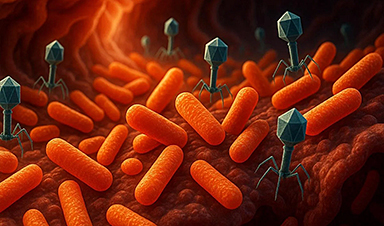
Scientists Flip a Gut Virus “Kill Switch” – Expose a Hidden Threat in Antibiotic Treatment
Scientists have long known that bacteriophages, viruses that infect bacteria, live in our gut, but exactly what they do has remained elusive. Researchers developed a clever mouse model that can temporarily eliminate these phages [...]
Enhanced Antibacterial Polylactic Acid-Curcumin Nanofibers for Wound Dressing
Background Wound healing is a complex physiological process that can be compromised by infection and impaired tissue regeneration. Conventional dressings, typically made from natural fibers such as cotton or linen, offer limited functionality. Nanofiber [...]
Global Nanomaterial Regulation: A Country-by-Country Comparison
Nanomaterials are materials with at least one dimension smaller than 100 nanometres (about 100,000 times thinner than a human hair). Because of their tiny size, they have unique properties that can be useful in [...]
Pandemic Potential: Scientists Discover 3 Hotspots of Deadly Emerging Disease in the US
Virginia Tech researchers discovered six new rodent carriers of hantavirus and identified U.S. hotspots, highlighting the virus’s adaptability and the impact of climate and ecology on its spread. Hantavirus recently drew public attention following reports [...]
Studies detail high rates of long COVID among healthcare, dental workers
Researchers have estimated approximately 8% of Americas have ever experienced long COVID, or lasting symptoms, following an acute COVID-19 infection. Now two recent international studies suggest that the percentage is much higher among healthcare workers [...]
Melting Arctic Ice May Unleash Ancient Deadly Diseases, Scientists Warn
Melting Arctic ice increases human and animal interactions, raising the risk of infectious disease spread. Researchers urge early intervention and surveillance. Climate change is opening new pathways for the spread of infectious diseases such [...]
Scientists May Have Found a Secret Weapon To Stop Pancreatic Cancer Before It Starts
Researchers at Cold Spring Harbor Laboratory have found that blocking the FGFR2 and EGFR genes can stop early-stage pancreatic cancer from progressing, offering a promising path toward prevention. Pancreatic cancer is expected to become [...]
Breakthrough Drug Restores Vision: Researchers Successfully Reverse Retinal Damage
Blocking the PROX1 protein allowed KAIST researchers to regenerate damaged retinas and restore vision in mice. Vision is one of the most important human senses, yet more than 300 million people around the world are at [...]
Differentiating cancerous and healthy cells through motion analysis
Researchers from Tokyo Metropolitan University have found that the motion of unlabeled cells can be used to tell whether they are cancerous or healthy. They observed malignant fibrosarcoma [...]