Researchers at UCLA have unveiled startling findings using PSMA-PET imaging that reveal nearly half of patients diagnosed with high-risk prostate cancer might actually have metastases missed by traditional imaging methods.
This revelation could profoundly affect future treatment decisions and patient outcomes, highlighting the necessity of incorporating advanced imaging technologies into standard diagnostic procedures.
Breakthroughs in Prostate Cancer Imaging
Researchers at UCLA Health’s Jonsson Comprehensive Cancer Center have discovered that many cases of high-risk, hormone-sensitive prostate cancer classified as nonmetastatic may actually be more advanced than originally believed.
The study, published today (January 3) in JAMA Network Open, revealed that nearly half of these patients, initially diagnosed as nonmetastatic using traditional imaging, were found to have metastatic disease when assessed with advanced prostate-specific membrane antigen–positron emission tomography (PSMA-PET) imaging. This suggests that conventional imaging often underestimates the extent of cancer spread.
Impact of PSMA-PET on Treatment Decisions
“Our study demonstrates the critical role of PSMA-PET in accurately staging prostate cancer, which can significantly impact treatment decisions and outcomes,” said senior author of the study Dr. Jeremie Calais, director of the Ahmanson Translational Theranostics Division’s clinical research program and associate professor at the department of molecular and medical pharmacology at the David Geffen School of Medicine at UCLA.
This advanced imaging technology plays a critical role in redefining how prostate cancer is staged. PSMA-PET imaging uses tiny amounts of radioactive “tracers,” called radiotracers, that binds to prostate cancer cells, making them visible on PET scans. Unlike conventional imaging, which provides only anatomical details, PSMA-PET offers functional imaging that reveals the cancer’s biological activity, which can significantly improve the accuracy of disease staging.
Changing Clinical Practices with New Imaging Techniques
The clinical adoption of PSMA-PET has changed the landscape of prostate cancer imaging, yet treatment decisions often rely on clinical trials that did not incorporate this advanced imaging technique for patient selection.
To better understand the advantages of PSMA-PET over conventional imaging, researchers conducted a post hoc, retrospective cross-sectional study using data from 182 patients with high-risk recurrent prostate cancers who were thought to have disease limited to the prostate and were eligible for the EMBARK trial.
This clinical trial previously demonstrated that adding enzalutamide, a type of hormone therapy, to androgen deprivation therapy significantly improves metastasis-free survival. However, the trial relied on conventional imaging to classify patients, which researchers believe might have underestimated the disease’s extent in some cases.
In the cohort of patients, the researchers found PSMA-PET detected cancer metastases in 46% of patients, even though traditional imaging had suggested no evidence of cancer spread. Based on PSMA-PET, 24% of the patients even showed 5 or more lesions that had been missed by conventional imaging.
“We anticipated that PSMA-PET would detect more suspicious findings compared to conventional imaging. However, it was informative to uncover such a high number of metastatic findings in a well-defined cohort of patients resembling the EMBARK trial population that was supposed to only include those without metastases,” said Dr. Adrien Holzgreve, a visiting assistant professor at the David Geffen School of Medicine and first author of the study.
Implications for Future Research and Clinical Trials
These results challenge the interpretation of previous studies, like the EMBARK trial, and support the inclusion of PSMA-PET for patient selection in clinical and trial interventions in prostate cancer in future major industry-sponsored clinical trials. It also highlights the need to reevaluate treatment strategies and opens the door to potentially curative options for some patients, such as targeted radiotherapy, while raising important questions about integrating new imaging technologies into standard care.
While the current findings underscore PSMA-PET’s potential, researchers are continuing to explore its broader applications through additional studies. More research is needed to understand its impact on long-term patient outcomes and how it can best guide therapy, noted Calais.
“We have good rationales to assume that it is helpful to primarily rely on PSMA-PET findings,” said Holzgreve. “But more high-quality prospective data would be needed to claim superiority of PSMA-PET for treatment-guidance in terms of patient outcome. However, we are confident PSMA-PET will continue to advance prostate cancer staging and guide personalized therapies.”
Ongoing efforts at UCLA include analyzing follow-up data from four UCLA trials to assess how PSMA-PET findings influenced treatment decisions and patient outcomes. Additionally, as part of an international consortium studying over 6,000 patients, the team is investigating the prognostic value of PSMA-PET.
Reference: 3 January 2025, JAMA Network Open.
DOI: 10.1001/jamanetworkopen.2024.52971
News
When You Lose Weight, Where Does It Actually Go?
Most health professionals lack a clear understanding of how body fat is lost, often subscribing to misconceptions like fat converting to energy or muscle. The truth is, fat is actually broken down into carbon [...]
How Everyday Plastics Quietly Turn Into DNA-Damaging Nanoparticles
The same unique structure that makes plastic so versatile also makes it susceptible to breaking down into harmful micro- and nanoscale particles. The world is saturated with trillions of microscopic and nanoscopic plastic particles, some smaller [...]
AI Outperforms Physicians in Real-World Urgent Care Decisions, Study Finds
The study, conducted at the virtual urgent care clinic Cedars-Sinai Connect in LA, compared recommendations given in about 500 visits of adult patients with relatively common symptoms – respiratory, urinary, eye, vaginal and dental. [...]
Challenging the Big Bang: A Multi-Singularity Origin for the Universe
In a study published in the journal Classical and Quantum Gravity, Dr. Richard Lieu, a physics professor at The University of Alabama in Huntsville (UAH), which is a part of The University of Alabama System, suggests that [...]
New drug restores vision by regenerating retinal nerves
Vision is one of the most crucial human senses, yet over 300 million people worldwide are at risk of vision loss due to various retinal diseases. While recent advancements in retinal disease treatments have [...]
Shingles vaccine cuts dementia risk by 20%, new study shows
A shingles shot may do more than prevent rash — it could help shield the aging brain from dementia, according to a landmark study using real-world data from the UK. A routine vaccine could [...]
AI Predicts Sudden Cardiac Arrest Days Before It Strikes
AI can now predict deadly heart arrhythmias up to two weeks in advance, potentially transforming cardiac care. Artificial intelligence could play a key role in preventing many cases of sudden cardiac death, according to [...]
NanoApps Medical is a Top 20 Feedspot Nanotech Blog
There is an ocean of Nanotechnology news published every day. Feedspot saves us a lot of time and we recommend it. We have been using it since 2018. Feedspot is a freemium online RSS [...]
This Startup Says It Can Clean Your Blood of Microplastics
This is a non-exhaustive list of places microplastics have been found: Mount Everest, the Mariana Trench, Antarctic snow, clouds, plankton, turtles, whales, cattle, birds, tap water, beer, salt, human placentas, semen, breast milk, feces, testicles, [...]
New Blood Test Detects Alzheimer’s and Tracks Its Progression With 92% Accuracy
The new test could help identify which patients are most likely to benefit from new Alzheimer’s drugs. A newly developed blood test for Alzheimer’s disease not only helps confirm the presence of the condition but also [...]
The CDC buried a measles forecast that stressed the need for vaccinations
This story was originally published on ProPublica, a nonprofit newsroom that investigates abuses of power. Sign up to receive our biggest stories as soon as they’re published. ProPublica — Leaders at the Centers for Disease Control and Prevention [...]
Light-Driven Plasmonic Microrobots for Nanoparticle Manipulation
A recent study published in Nature Communications presents a new microrobotic platform designed to improve the precision and versatility of nanoparticle manipulation using light. Led by Jin Qin and colleagues, the research addresses limitations in traditional [...]
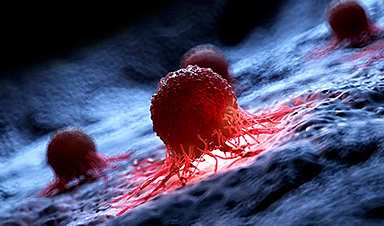
Cancer’s “Master Switch” Blocked for Good in Landmark Study
Researchers discovered peptides that permanently block a key cancer protein once thought untreatable, using a new screening method to test their effectiveness inside cells. For the first time, scientists have identified promising drug candidates [...]
AI self-cloning claims: A new frontier or a looming threat?
Chinese scientists claim that some AI models can replicate themselves and protect against shutdown. Has artificial intelligence crossed the so-called red line? Chinese researchers have published two reports on arXiv claiming that some artificial [...]
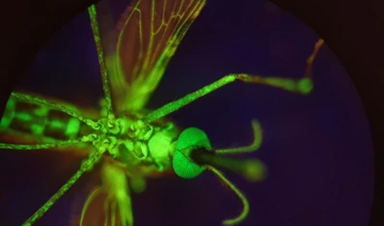
New Drug Turns Human Blood Into Mosquito-Killing Weapon
Nitisinone, a drug for rare diseases, kills mosquitoes when present in human blood and may become a new tool to fight malaria, offering longer-lasting, environmentally safer effects than ivermectin. Controlling mosquito populations is a [...]
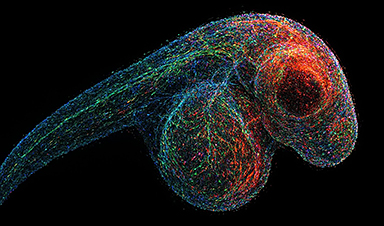
DNA Microscopy Creates 3D Maps of Life From the Inside Out
What if you could take a picture of every gene inside a living organism—not with light, but with DNA itself? Scientists at the University of Chicago have pioneered a revolutionary imaging technique called volumetric DNA microscopy. It builds [...]