When COVID-19 spread around the globe this year, David Montefiori wondered how the deadly virus behind the pandemic might be changing as it passed from person to person. Montefiori is a virologist who has spent much of his career studying how chance mutations in HIV help it to evade the immune system. The same thing might happen with SARS-CoV-2, he thought.
In March, Montefiori, who directs an AIDS-vaccine research laboratory at Duke University in Durham, North Carolina, contacted Bette Korber, an expert in HIV evolution and a long-time collaborator. Korber, a computational biologist at the Los Alamos National Laboratory (LANL) in Sante Fe, New Mexico, had already started scouring thousands of coronavirus genetic sequences for mutations that might have changed the virus’s properties as it made its way around the world.
Compared with HIV, SARS-CoV-2 is changing much more slowly as it spreads. But one mutation stood out to Korber. It was in the gene encoding the spike protein, which helps virus particles to penetrate cells. Korber saw the mutation appearing again and again in samples from people with COVID-19. At the 614th amino-acid position of the spike protein, the amino acid aspartate (D, in biochemical shorthand) was regularly being replaced by glycine (G) because of a copying fault that altered a single nucleotide in the virus’s 29,903-letter RNA code. Virologists were calling it the D614G mutation.
In April, Korber, Montefiori and others warned in a preprint posted to the bioRxiv server that “D614G is increasing in frequency at an alarming rate”1. It had rapidly become the dominant SARS-CoV-2 lineage in Europe and had then taken hold in the United States, Canada and Australia. D614G represented a “more transmissible form of SARS-CoV-2”, the paper declared, one that had emerged as a product of natural selection.
Image Credit: Closed’ and ‘open’ conformations of the spike protein on SARS-CoV-2, which binds to receptors on human cells. A common mutation (circled) seems to make the protein favour open conformations, which might mean the virus can enter cells more easily.
Structural data from K. Shen & J. Luban
Post by Amanda Scott, NA CEO. Follow her on twitter @tantriclens
Thanks to Heinz V. Hoenen. Follow him on twitter: @HeinzVHoenen
News
According to Researchers, Your Breathing Patterns Could Hold the Key to Better Memory
Breathing synchronizes brain waves that support memory consolidation. A new study from Northwestern Medicine reports that, much like a conductor harmonizes various instruments in an orchestra to create a symphony, breathing synchronizes hippocampal brain waves to [...]
The Hidden Culprit Behind Alzheimer’s Revealed: Microglia Under the Microscope
Researchers at the CUNY Graduate Center have made a groundbreaking discovery in Alzheimer’s disease research, identifying a critical link between cellular stress in the brain and disease progression. Their study focuses on microglia, the brain’s immune [...]
“Mirror Bacteria” Warning: A New Kind of Life Could Pose a Global Threat
Mirror life, a concept involving synthetic organisms with reversed molecular structures, carries significant risks despite its potential for medical advancements. Experts warn that mirror bacteria could escape natural biological controls, potentially evolving to exploit [...]
Lingering Viral Fragments: The Hidden Cause of Long COVID
Long COVID, affecting 5-10% of COVID-19 patients, might be caused by the enduring presence of the virus in the body. Research suggests that viral fragments, possibly live, linger and lead to symptoms. Addressing this involves antiviral treatments, enhanced [...]
Hidden Scars: How COVID Lockdowns Altered Teen Brains Forever
Research from the University of Washington revealed that COVID-19 lockdowns led to accelerated cortical thinning in adolescents, impacting brain development significantly. This effect was more pronounced in females than males, raising concerns about long-term brain health. The study [...]
Simple Blood Test To Detect Dementia Before Symptoms Appear
UCLA researchers have identified placental growth factor (PlGF) as a potential blood biomarker for early detection of cognitive impairment and dementia. High PlGF levels correlate with increased vascular permeability, suggesting its role in the development [...]
Investing Goldman Sachs asks ‘Is curing patients a sustainable business model?’
Goldman Sachs analysts attempted to address a touchy subject for biotech companies, especially those involved in the pioneering “gene therapy” treatment: cures could be bad for business in the long run. “Is curing patients [...]
The risks of reversed chirality: Study highlights dangers of mirror organisms
A groundbreaking study evaluates the feasibility, risks, and ethical considerations of creating mirror bacteria with reversed chirality, highlighting potential threats to health and ecosystems. In a recent study published in Science, a team of researchers [...]
Alarming Mutation in H5N1 Virus Raises Pandemic Red Flags
NIH-funded study concludes that the risk of human infection remains low A recent study published in Science and funded by the National Institutes of Health (NIH) has found that a single alteration in a protein on the surface [...]
Scientists Discover Genetic Changes Linked to Autism, Schizophrenia
The Tbx1 gene influences brain volume and social behavior in autism and schizophrenia, with its deficiency linked to amygdala shrinkage and impaired social incentive evaluation. A study published in Molecular Psychiatry has linked changes in brain [...]
How much permafrost will melt this century, and where will its carbon go?
Among the many things global warming will be melting this century—sea ice, land glaciers and tourist businesses in seaside towns across the world—is permafrost. Lying underneath 15% of the northern hemisphere, permafrost consists of [...]
A Physics Discovery So Strange It’s Changing Quantum Theory
MIT physicists surprised to discover electrons in pentalayer graphene can exhibit fractional charge. New theoretical research from MIT physicists explains how it could work, suggesting that electron interactions in confined two-dimensional spaces lead to novel quantum states, [...]
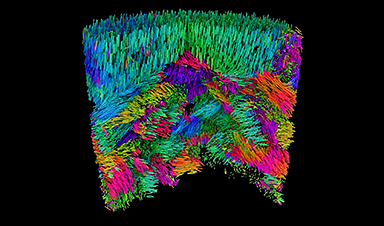
Inside the Nano-Universe: New 3D X-Ray Imaging Transforms Material Science
A cutting-edge X-ray method reveals the 3D orientation of nanoscale material structures, offering fresh insights into their functionality. Researchers at the Swiss Light Source (SLS) have developed a groundbreaking technique called X-ray linear dichroic orientation tomography [...]
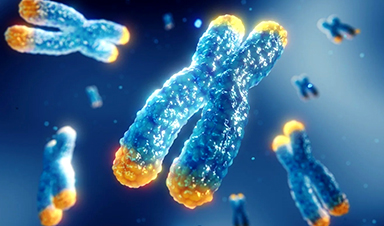
X-chromosome study reveals hidden genetic links to Alzheimer’s disease
Despite decades of research, the X-chromosome’s impact on Alzheimer’s was largely ignored until now. Explore how seven newly discovered genetic loci could revolutionize our understanding of the disease. Conventional investigations of the genetic contributors [...]
The Unresolved Puzzle of Long COVID: 30% of Young People Still Suffer After Two Years
A UCL study found that 70% of young people with long Covid recovered within 24 months, but recovery was less likely among older teenagers, females, and those from deprived backgrounds. Researchers emphasized the need [...]
Needle-Free: New Nano-Vaccine Effective Against All COVID-19 Variants
A new nano-vaccine developed by TAU and the University of Lisbon offers a needle-free, room-temperature-storable solution against COVID-19, targeting all key variants effectively. Professor Ronit Satchi-Fainaro’s lab at Tel Aviv University’s Faculty of Medical and [...]