Understanding rare diseases
Rare diseases affect less than 5 people out of 10,000. However, this still amounts to about 7% of the world’s population, with over 10,000 such conditions. Almost all are genetic in origin, with a few being autoimmune or infectious.
Most such patients undergo a diagnostic and therapeutic odyssey involving extensive and prolonged testing and multiple consultations. Only about 5% of rare diseases are currently treatable, the rest being “orphan diseases.” However, precision medicine could provide an answer to this problem.
Precision medicine and rare diseases
Precision medicine may be described as treatment tailored to the individual patient, based on detailed data about the patient coupled with reasoning back to the root cause at the molecular level. It aims at maximum therapeutic efficacy and minimal drug toxicity for all diseases. It accounts for inter-individual genetic variation that makes each person respond differently to a given disease or its treatment.
Genetic and molecular profiling
Personalized diagnostics
Advances in genomic sequencing, data science, imaging techniques, and genetic diagnosis have made it feasible to study orphan diseases in individual patients or small numbers of patients with a single rare disease. The development of precision medicine added economic and scientific value to investments in this field.
With rare diseases, identification of the molecular pathology, whether an abnormal gene or metabolic pathway, occurs simultaneously with the diagnosis. This should theoretically facilitate treatment since all that is needed is the correction of the single molecular flaw.
The challenge
Traditionally, pharmaceutical research has focused on finding and developing commercially viable treatments that benefit large groups of people, thus excluding people with rare diseases. Few rare diseases have at least one or two approved treatments, leaving a large and untapped market for personalized therapies – mostly gene and cell therapies.
The promise
Whole-genome sequencing and whole-exome sequencing have overcome some important limitations of earlier genomics platforms, enabling the identification of many more pathogenic genetic defects, while RNA sequencing extends its reach.
Still, vast regions of non-coding DNA may contain pathogenic mutations, including regulatory elements, the 5′ untranslated region (5′UTR), and epigenetic modifications. Genome-wide association studies (GWAS), along with transcriptomics, have helped identify genotype-phenotype associations.
Large datasets and data-sharing networks are vital to identifying rare disease gene variants. In the USA, the NIH Undiagnosed Diseases Network (UDN) used an earlier program’s searchable clinical and exome sequencing database to help patients undergoing a diagnostic odyssey reach a diagnosis while gathering valuable data. The UDN assessed over 1,000 patients with one week of hospitalization, diagnosing over 200 very rare diseases and discovering new diseases.
Achieving Rare Disease Research Goals with MGI
This has been extended to UDN International at present, one of several international organizations such as Care-for-Rare, REACT, and IRDIRC that help children with rare diseases.
Tailoring treatments for rare diseases
Customized therapies
Rare disease researchers use gene knock-out and drug repurposing screens in cell lines, tissue models, or animal lines to understand how mutations and drugs affect different cell types, including safety, tolerability, and bioavailability thresholds. This not only identifies diverse drug and gene targets but also allows for optimal treatment design in orphan diseases.
Success stories
1. SMA
The number one cause of death in babies worldwide is spinal muscle atrophy (SMA), caused by defective SMN1 genes leading to dysfunctional survival motor neuron (SMN) protein. This causes motor neuron breakdown and paralysis.
The first approved (2016) therapy for SMA is an ASO called Spinraza (nusinersen), which reduced deaths and the need for ventilation among SMA children. Injected intrathecally, Spinraza rescues motor neurons by promoting the production of functional SMN protein. Gene therapy is in the pipeline, and almost all other therapies are being developed.
2. Other neurological syndromes
Mila Makovec, in Colorado’s Longmont, had Batten’s disease and was rapidly deteriorating when she was put on a personalized nusinersen-like ASO, Milasen, starting in January 2018, to reactivate the single normal copy of the gene that she possessed. Within a month, her seizures were reduced by 50%, but she remains severely disabled.
Susannah Lorem had a rare genetic mutation, KIF1A, causing progressive, debilitating disease. The firm nLorem provided a personalized ASO free for life, starting October 2022.
3. Duchenne
Hereditary muscular disease called Duchenne muscular dystrophy (DMD) causes progressive muscle weakness caused by abnormalities in the dystrophin (a muscle protein) gene. It affects less than one in 6,000 male babies each year.
Potential therapies for DMD include ataluren, a small molecule that causes exon skipping. This could reverse the effect of a nonsense mutation disrupting dystrophin synthesis. That is, it skips a premature stop codon, allowing dystrophin gene transcription.
Sarepta Therapeutics has launched a one-time gene therapy for DMD that enables functional dystrophin synthesis. However, adverse effects, such as acute severe liver injury, myositis, and myocarditis, have been reported during the clinical trials, and a post-marketing trial is going on.
Investigational gene therapies from Pfizer are showing immense promise in DMD, with improvements lasting about 3-5 years.
4. Cystic Fibrosis
Cystic fibrosis (CF) patients rarely live beyond early childhood. Though discovered in 1980, the CFTR gene has 2,000 pathogenic variants, making gene therapy an unsolved challenge in this case. Small-molecule drugs called CFTR modulators have been launched to correct defective CFTR protein function.
An oral drug, Trikafta, combines 3 CFTR modulators, reversing the effects of 178 different CFTR mutations. It may prolong survival in about 90% of CF patients.
The average CF patient lives ten times as long today as in any previous era, with a lifespan extending into the fifties. Notably, this is also because of intensive collaborative research resulting in better airway and nutritional management and improved antibiotic therapy, besides the CFTR modulators.
Challenges and future directions
Overcoming hurdles
Ethical principles still being discussed include the high cost of treating a single individual vs the cost of treating large numbers with readily available drugs. Other questions include the type of evidence needed for drug approval in humans and how to assess its efficacy.
There are nowhere near enough researchers to make custom drugs for all who might want them. And even if there were, who would pay? Unfortunately, that leaves it to families,” says Dr. Steven Joffe, a medical ethicist at the University of Pennsylvania.
Since the Orphan Drug Act of 1983 became law in the United States, research into rare disease therapies has accelerated. The key shift is in value, making rare disease research a booming industry, with the market expected to grow by over 10% every year.
The large market base, plus the incentives from government and private investors such as early access, expanded access, accelerated approval, and extended patent rights programs, coupled with the fact that cell and gene therapies are at the heart of treatment for rare diseases, have powerfully stimulated research and development. In fact, these treatments are readily commercialized despite the small number of patients.
Drug repurposing studies identified the already approved drug epalrestat as a potential therapy for the rare disease PMM2-CDG, a glycosylation disorder. This was followed by a successful trial in the index individual, and larger trials are ongoing.
Rational therapeutic design is a tool to identify molecules that reverse the undesirable impact caused by a pathogenic genetic variant. This helped to identify low-dose ketamine as a potential therapy for a rare disease, ADNP syndrome, part of the autism spectrum disorder.
Precision Medicine in the Era of Rare, 2024
This method includes enzyme replacement in cases of metabolic errors like Gaucher’s disease, antisense oligonucleotides (ASO), tiny corrective DNA bits for spinal muscular atrophy (SMA), small-molecule drugs for cystic fibrosis, and cell or gene-based therapies like stem cell gene therapy for adenosine deaminase deficiency.
Advances in stem cell research help assess individual responses to drugs and identify specific mutations that respond to potentially engineered therapies. This will maximize the odds of obtaining the desired response in clinical practice.
CRISPR gene editing-based therapies to eliminate pathogenic genes with point mutations as in sickle cell disease, and viral gene delivery vectors, are being investigated. Many issues remain to be overcome before their clinical launch.
Using sophisticated data analytics and artificial intelligence (AI) on large datasets of people, either orphan disease patients or related in some way, firms have helped educate and sensitize patients and healthcare providers in the most relevant ways. Such data can help identify high-risk regions or populations, increasing by up to 40% the number of potential patients found.
Using real-world data from large datasets, firms can take advantage of accelerated approval programs for orphan drugs by showing associations between rare diseases and life-threatening outcomes, which could not be proved from the small number of patients available by traditional methods.
Digital technology, including mobile apps, can be leveraged to educate and support patients and caregivers after the diagnosis. It can help HCPs track symptoms and optimize treatment schedules for such patients.
Pharmaceutical companies may invest in such support services in return for real-world information on how their therapies affect the patient. The high costs of treatment, coupled with the need for frequent traveling and doctor appointments, are daunting for many such patients, presenting another opportunity for health investors to step in.
References
- Might, M. et al. (2022). Why rare disease needs precision medicine—and precision medicine needs rare disease. Cell Reports Medicine. doi: https://doi.org/10.1016/j.xcrm.2022.100530. https://www.cell.com/cell-reports-medicine/fulltext/S2666-3791(22)00030-1.
- Villalon-Garcia, I. et al. (2020). Precision Medicine in Rare Diseases. Diseases. doi: https://doi.org/10.3390%2Fdiseases8040042. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7709101/.
- Treating rare diseases: How digital technologies can drive innovation. (2024). https://www.mckinsey.com/industries/life-sciences/our-insights/treating-rare-diseases-how-digital-technologies-can-drive-innovation.
- Shan, Z. et al. (2022). Medical care of rare and undiagnosed diseases: Prospects and challenges. Fundamental Research. https://doi.org/10.1016/j.fmre.2022.08.018. https://www.sciencedirect.com/science/article/pii/S2667325822003594.
- Ligezka, A. N. et al. (2021). Sorbitol Is a Severity Biomarker for PMM2-CDG with Therapeutic Implications. Annals of Neurology. https://doi.org/10.1002%2Fana.26245. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8820356/.
- Luxner, L. (2023). Pfizer gene therapy shows huge promise for boys with dmd, but questions loom. Rare Disease Advisor. https://www.rarediseaseadvisor.com/features/pfizer-gene-therapy-shows-promise-boys-dmd-questions-loom/.
- Ozkaya, O. (2023). FDA approves first gene therapy for DMD. Rare Disease Advisor. https://www.rarediseaseadvisor.com/news/dmd-news-briefs/fda-approves-first-gene-therapy-dmd/.
- Elborn, S. (2018). The history, and the future, of cystic fibrosis. https://www.rbht.nhs.uk/blog/history-and-future-cystic-fibrosis.
- Prakash, V. (2017). Spinraza—a rare disease success story. Gene Therapy. doi: https://doi.org/10.1038/gt.2017.59. https://www.nature.com/articles/gt201759.
- Klein, C. et al. (2018). Patients with rare diseases: from therapeutic orphans to pioneers of personalized treatments. EMBO Molecular Medicine. doi: https://doi.org/10.15252%2Femmm.201708365. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5760852/.
- Susannah’s Story. https://www.nlorem.org/susannahs-story/. Retrieved on 24 January, 2024.
- Scientists Designed a Drug for Just One Patient. Her Name Is Mila. https://www.nytimes.com/2019/10/09/health/mila-makovec-drug.html. Retrieved on 24 January, 2024.
- Kim, J. et al. (2019). Patient-Customized Oligonucleotide Therapy for a Rare Genetic Disease. New England Journal of Medicine. doi: 10.1056/NEJMoa1813279. https://www.nejm.org/doi/full/10.1056/NEJMoa1813279.
News
Chernobyl scientists discover black fungus feeding on deadly radiation
It looks pretty sinister, but it might actually be incredibly helpful When reactor number four in Chernobyl exploded, it triggered the worst nuclear disaster in history, one which the surrounding area still has not [...]
Long COVID Is Taking A Silent Toll On Mental Health, Here’s What Experts Say
Months after recovering from COVID-19, many people continue to feel unwell. They speak of exhaustion that doesn’t fade, difficulty breathing, or an unsettling mental haze. What’s becoming increasingly clear is that recovery from the [...]
Study Delivers Cancer Drugs Directly to the Tumor Nucleus
A new peptide-based nanotube treatment sneaks chemo into drug-resistant cancer cells, providing a unique workaround to one of oncology’s toughest hurdles. CiQUS researchers have developed a novel molecular strategy that allows a chemotherapy drug to [...]
Scientists Begin $14.2 Million Project To Decode the Body’s “Hidden Sixth Sense”
An NIH-supported initiative seeks to unravel how the nervous system tracks and regulates the body’s internal organs. How does your brain recognize when it’s time to take a breath, when your blood pressure has [...]
Scientists Discover a New Form of Ice That Shouldn’t Exist
Researchers at the European XFEL and DESY are investigating unusual forms of ice that can exist at room temperature when subjected to extreme pressure. Ice comes in many forms, even when made of nothing but water [...]
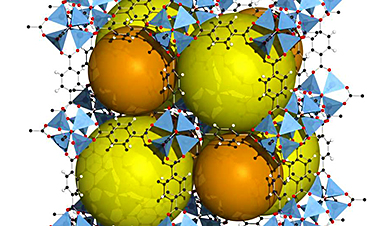
Nobel-winning, tiny ‘sponge crystals’ with an astonishing amount of inner space
The 2025 Nobel Prize in chemistry was awarded to Richard Robson, Susumu Kitagawa and Omar Yaghi on Oct. 8, 2025, for the development of metal-organic frameworks, or MOFs, which are tunable crystal structures with extremely [...]
Harnessing Green-Synthesized Nanoparticles for Water Purification
A new review reveals how plant- and microbe-derived nanoparticles can power next-gen water disinfection, delivering cleaner, safer water without the environmental cost of traditional treatments. A recent review published in Nanomaterials highlights the potential of green-synthesized nanomaterials (GSNMs) in [...]
Brainstem damage found to be behind long-lasting effects of severe Covid-19
Damage to the brainstem - the brain's 'control center' - is behind long-lasting physical and psychiatric effects of severe Covid-19 infection, a study suggests. Using ultra-high-resolution scanners that can see the living brain in [...]
CT scan changes over one year predict outcomes in fibrotic lung disease
Researchers at National Jewish Health have shown that subtle increases in lung scarring, detected by an artificial intelligence-based tool on CT scans taken one year apart, are associated with disease progression and survival in [...]
AI Spots Hidden Signs of Disease Before Symptoms Appear
Researchers suggest that examining the inner workings of cells more closely could help physicians detect diseases earlier and more accurately match patients with effective therapies. Researchers at McGill University have created an artificial intelligence tool capable of uncovering [...]
Breakthrough Blood Test Detects Head and Neck Cancer up to 10 Years Before Symptoms
Mass General Brigham’s HPV-DeepSeek test enables much earlier cancer detection through a blood sample, creating a new opportunity for screening HPV-related head and neck cancers. Human papillomavirus (HPV) is responsible for about 70% of [...]
Study of 86 chikungunya outbreaks reveals unpredictability in size and severity
The symptoms come on quickly—acute fever, followed by debilitating joint pain that can last for months. Though rarely fatal, the chikungunya virus, a mosquito-borne illness, can be particularly severe for high-risk individuals, including newborns and older [...]
Tiny Fat Messengers May Link Obesity to Alzheimer’s Plaque Buildup
Summary: A groundbreaking study reveals how obesity may drive Alzheimer’s disease through tiny messengers called extracellular vesicles released from fat tissue. These vesicles carry lipids that alter how quickly amyloid-β plaques form, a hallmark of [...]
Ozone exposure weakens lung function and reshapes the oral microbiome
Scientists reveal that short-term ozone inhalation doesn’t just harm the lungs; it reshapes the microbes in your mouth, with men facing the greatest risks. Ozone is a toxic environmental pollutant with wide-ranging effects on [...]
New study reveals molecular basis of Long COVID brain fog
Even though many years have passed since the start of the COVID-19 pandemic, the effects of infection with SARS-CoV-2 are not completely understood. This is especially true for Long COVID, a chronic condition that [...]
Scientists make huge Parkinson’s breakthrough as they discover ‘protein trigger’
Scientists have, for the first time, directly visualised the protein clusters in the brain believed to trigger Parkinson's disease, bringing them one step closer to potential treatments. Parkinson's is a progressive incurable neurological disorder [...]