Pancreatic cancer reprograms nerve cells to fuel its growth, but blocking these connections can shrink tumors and boost treatment effectiveness.
Pancreatic cancer is closely linked to the nervous system, according to researchers from the German Cancer Research Center (DKFZ) and the Heidelberg Institute for Stem Cell Technology and Experimental Medicine (HI-STEM). Their recent study, published in Nature, reveals that pancreatic tumors actively reprogram neurons to support their growth.
In experiments with mice, the researchers found that blocking nerve function not only slowed tumor progression but also made cancer cells more responsive to certain chemotherapy and immunotherapy treatments.
Over the past several years, scientists have observed interactions between cancer and the nervous system in nearly all studied tumor types, often finding that these interactions help tumors grow and survive. Pancreatic cancer, in particular, is surrounded by a dense network of nerves. However, only nerve fibers extend into the tumor, while the main bodies of the nerve cells remain in distant ganglia, the control centers of the peripheral nervous system. Until now, the exact molecular interactions between these nerves and cancer cells remained unclear.
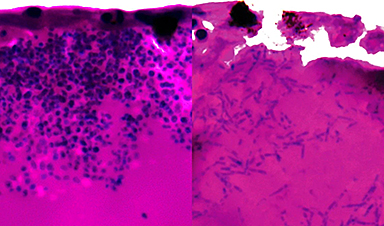
Using a newly developed method, a team led by Andreas Trumpp, DKFZ, and HI-STEM, has now succeeded for the first time in molecularly examining the nerve cells in both healthy tissue and pancreatic cancer in mice.
Pancreatic cancer reprograms nerve cells
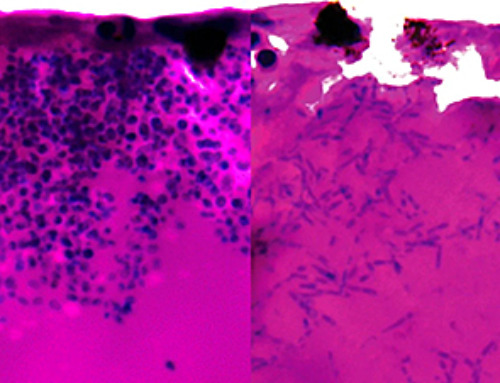
In pancreatic tumors, the nerves are extremely well-ramified and in contact with most of the tumor cells. Through the detailed molecular analysis of the individual neurons in the tumor, the researchers discovered that pancreatic cancer reprograms the gene activity of the nerves for its own benefit. The activity of many genes is increased or attenuated, resulting in a tumor-specific signature.
What is more, even after surgical removal of the primary tumor, the tumor nervous system retained its cancer-promoting properties: when the scientists reimplanted pancreatic cancer cells into the animals that had undergone surgery, the resulting secondary tumors were twice as large as those of mice that had been transplanted with pancreatic cancer cells for the first time.
In addition to their direct interaction with cancer cells, nerve cells influence in particular the fibroblasts of the tumor (CAF – cancer-associated fibroblasts), which make up a large part of the tumor mass. They are also stimulated to grow and contribute significantly to the suppression of the immune defense in the tumor environment.
Nerves cut – tumors shrink
When the sympathetic nerve connections to the pancreas were surgically severed or destroyed with special neurotoxins, tumor growth was significantly inhibited. At the same time, the activity of growth-promoting genes in the cancer cells as well as in the CAFs decreased. In the CAFs, the researchers observed a significant increase in pro-inflammatory gene activity after the nerves were destroyed.
“Apparently, the neuronal connections in pancreatic cancer suppress the pro-inflammatory activity of the fibroblasts, thereby inhibiting the cancer defense by immune cells,” explains Vera Thiel, the first author of the paper.
Severed nerves increase the effectiveness of immunotherapies
If the interruption of nerve connections apparently has an inflammatory effect, i.e. activates the immune system, this could increase the effectiveness of an immunotherapy with so-called checkpoint inhibitors (ICI). Drugs in this group metaphorically speaking release the “brakes” of the immune system. However, they cannot combat pancreatic carcinomas on their own: the tumors are considered immunologically “cold”, meaning the therapeutically important T-cells simply cannot reach the tumor.
When the researchers blocked the neural connection to the pancreatic tumor in a mouse model using a targeted neurotoxin, the tumor became sensitive to the checkpoint inhibitor nivolumab again and the tumor mass shrank to one-sixth of the mass in control animals. “By blocking the nerves, were able to convert an immunologically cold tumor into one that was sensitive to immunotherapy,” says Simon Renders, also a first author of the publication, summarizing the result.
Severed nerves plus chemotherapy: synergistic effect
The drug nab-paclitaxel is a component of standard chemotherapy for pancreatic cancer. In addition to inhibiting cell division, it also affects sensory nerves, which is why peripheral neuropathy is one of the known severe side effects of this agent.
Trumpp’s team showed that under repeated cycles of nab-paclitaxel, the sensory nerve fibers in the tumor decreased drastically. The tumor mass also decreased as expected. The effect on sensory nerves apparently seems to be part of the drug’s effectiveness against pancreatic cancer. However, the remaining nerve fibers retained their cancer-promoting gene activity even under treatment.
But what happens when the tumor is completely cut off from its neuronal connections? The researchers achieved this by treating the mice with nab-paclitaxel (to block sensory nerves) and a neurotoxin to switch off the sympathetic neurons. This combination had a synergistic effect and reduced the tumor mass by more than 90 percent.
“The result underscores that both types of nerve cells have functional relevance for tumor growth,” explains Vera Thiel. ”Complete blockade of the communication between nerves and tumor in combination with chemotherapy and/or immune checkpoint inhibitors is a promising approach for combating pancreatic cancer more effectively in the future. For example, it is conceivable to reduce the size of the tumors to such an extent that they subsequently become resectable, Trumpp summarizes. His team, together with doctors from Heidelberg University Hospital, is already planning early clinical trials to test this strategy in pancreatic cancer patients.
The Heidelberg Institute for Stem Cell Research and Experimental Medicine (HI-STEM) gGmbH was founded in 2008 as a public-private partnership between the DKFZ and the Dietmar Hopp Foundation and has been funded by the foundation for 15 years now.
Why research in mice is necessary for this research project
To investigate which different types of peripheral nerves influence the development of pancreatic cancer, the fully developed nervous system of an intact organism is essential. In addition, the aim of the work was to examine the interaction between the nervous system and the tumor as a potential target for new therapeutic approaches. In order to discover possible synergies with the body’s own defense system, the immune system with all its components is also needed. Both cannot be reproduced in cell or organ culture systems.
Reference: “Characterization of single neurons reprogrammed by pancreatic cancer” by Vera Thiel, Simon Renders, Jasper Panten, Nicolas Dross, Katharina Bauer, Daniel Azorin, Vanessa Henriques, Vanessa Vogel, Corinna Klein, Aino-Maija Leppä, Isabel Barriuso Ortega, Jonas Schwickert, Iordanis Ourailidis, Julian Mochayedi, Jan-Philipp Mallm, Carsten Müller-Tidow, Hannah Monyer, John Neoptolemos, Thilo Hackert, Oliver Stegle, Duncan T. Odom, Rienk Offringa, Albrecht Stenzinger, Frank Winkler, Martin Sprick and Andreas Trumpp, 17 February 2025, Nature.
DOI: 10.1038/s41586-025-08735-3
News
We May Never Know if AI Is Conscious, Says Cambridge Philosopher
As claims about conscious AI grow louder, a Cambridge philosopher argues that we lack the evidence to know whether machines can truly be conscious, let alone morally significant. A philosopher at the University of [...]
AI Helped Scientists Stop a Virus With One Tiny Change
Using AI, researchers identified one tiny molecular interaction that viruses need to infect cells. Disrupting it stopped the virus before infection could begin. Washington State University scientists have uncovered a method to interfere with a key [...]
Deadly Hospital Fungus May Finally Have a Weakness
A deadly, drug-resistant hospital fungus may finally have a weakness—and scientists think they’ve found it. Researchers have identified a genetic process that could open the door to new treatments for a dangerous fungal infection [...]
Fever-Proof Bird Flu Variant Could Fuel the Next Pandemic
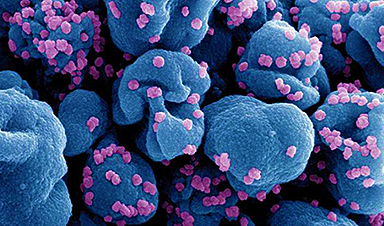
Bird flu viruses present a significant risk to humans because they can continue replicating at temperatures higher than a typical fever. Fever is one of the body’s main tools for slowing or stopping viral [...]
What could the future of nanoscience look like?
Society has a lot to thank for nanoscience. From improved health monitoring to reducing the size of electronics, scientists’ ability to delve deeper and better understand chemistry at the nanoscale has opened up numerous [...]
Scientists Melt Cancer’s Hidden “Power Hubs” and Stop Tumor Growth
Researchers discovered that in a rare kidney cancer, RNA builds droplet-like hubs that act as growth control centers inside tumor cells. By engineering a molecular switch to dissolve these hubs, they were able to halt cancer [...]
Platelet-inspired nanoparticles could improve treatment of inflammatory diseases
Scientists have developed platelet-inspired nanoparticles that deliver anti-inflammatory drugs directly to brain-computer interface implants, doubling their effectiveness. Scientists have found a way to improve the performance of brain-computer interface (BCI) electrodes by delivering anti-inflammatory drugs directly [...]
After 150 years, a new chapter in cancer therapy is finally beginning
For decades, researchers have been looking for ways to destroy cancer cells in a targeted manner without further weakening the body. But for many patients whose immune system is severely impaired by chemotherapy or radiation, [...]
Older chemical libraries show promise for fighting resistant strains of COVID-19 virus
SARS‑CoV‑2, the virus that causes COVID-19, continues to mutate, with some newer strains becoming less responsive to current antiviral treatments like Paxlovid. Now, University of California San Diego scientists and an international team of [...]
Lower doses of immunotherapy for skin cancer give better results, study suggests
According to a new study, lower doses of approved immunotherapy for malignant melanoma can give better results against tumors, while reducing side effects. This is reported by researchers at Karolinska Institutet in the Journal of the National [...]
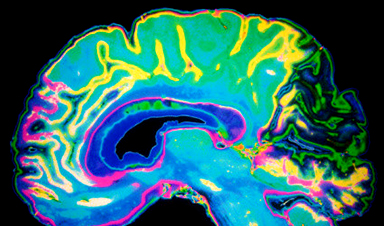
Researchers highlight five pathways through which microplastics can harm the brain
Microplastics could be fueling neurodegenerative diseases like Alzheimer's and Parkinson's, with a new study highlighting five ways microplastics can trigger inflammation and damage in the brain. More than 57 million people live with dementia, [...]
Tiny Metal Nanodots Obliterate Cancer Cells While Largely Sparing Healthy Tissue
Scientists have developed tiny metal-oxide particles that push cancer cells past their stress limits while sparing healthy tissue. An international team led by RMIT University has developed tiny particles called nanodots, crafted from a metallic compound, [...]
Gold Nanoclusters Could Supercharge Quantum Computers
Researchers found that gold “super atoms” can behave like the atoms in top-tier quantum systems—only far easier to scale. These tiny clusters can be customized at the molecular level, offering a powerful, tunable foundation [...]
A single shot of HPV vaccine may be enough to fight cervical cancer, study finds
WASHINGTON -- A single HPV vaccination appears just as effective as two doses at preventing the viral infection that causes cervical cancer, researchers reported Wednesday. HPV, or human papillomavirus, is very common and spread [...]
New technique overcomes technological barrier in 3D brain imaging
Scientists at the Swiss Light Source SLS have succeeded in mapping a piece of brain tissue in 3D at unprecedented resolution using X-rays, non-destructively. The breakthrough overcomes a long-standing technological barrier that had limited [...]
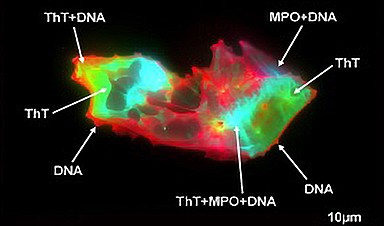
Scientists Uncover Hidden Blood Pattern in Long COVID
Researchers found persistent microclot and NET structures in Long COVID blood that may explain long-lasting symptoms. Researchers examining Long COVID have identified a structural connection between circulating microclots and neutrophil extracellular traps (NETs). The [...]