Research indicates hospitals contribute to the local spread of antibiotic-resistant infections.
A recent study published in the journal Infection Control & Hospital Epidemiology by the Society for Healthcare Epidemiology of America suggests that family members of patients discharged from hospitals may be at an increased risk of contracting antibiotic-resistant infections, commonly referred to as superbugs. This risk persists even if the patient themselves was not diagnosed with such an infection, indicating that hospitals may contribute to the spread of resistant bacteria in the community.
When recently hospitalized patients were diagnosed with the superbug — Methicillin-resistant Staphylococcus aureus infection (MRSA) — the risk to relatives living with them was even higher. The longer the relative’s hospital stay, even without a MRSA diagnosis, the higher the risk to family members.
“Patients can become colonized with MRSA during their hospital stay and transmit MRSA to their household members,” said Aaron Miller, PhD, lead researcher on the study and research assistant professor of internal medicine-infectious diseases at the University of Iowa. “This suggests hospitals contribute to the spread of MRSA into the community through discharged patients who are asymptomatic carriers.”
Recommendations for Hospitals
Miller recommends hospitals enhance infection control practices, including testing for MRSA colonization, especially at discharge, even with there are no symptoms of infection. He said MRSA colonization and infections could be tracked among hospital patients and their household contacts to identify and mitigate transmission more effectively.
“This important study illustrates the risk of spread of resistant pathogens related to healthcare and highlights the essential importance of core infection practices,” said SHEA President Thomas Talbot, M.D., chief hospital epidemiologist at Vanderbilt University Medical center. Talbot was not involved with the research. “Hand hygiene, environmental cleaning, and standard interventions to reduce Staphylococcal colonization are crucial to preventing the spread of resistant bacteria in healthcare settings.”
Understanding MRSA
MRSA infections are known as superbugs because they do not respond to common antibiotics, making them difficult to treat. MRSA generally occurs in people who have been in a hospital or another healthcare setting, such as a nursing home, but MRSA also spreads in communities outside the hospital, usually through skin-to-skin contact. Most people with MRSA have no symptoms, but the bacteria can cause painful swelling if it gets under the skin, and it can be deadly if it spreads to other parts of the body, such as blood or lungs.
Researchers used a large database of insurance claims that included 158 million enrollees with two or more family members on the same plan to learn about how MRSA spread after someone in a household had been in the hospital.
Reviewing 424,512 MRSA cases among 343,524 insured people, the study found 4,724 cases of MRSA being potentially transmitted to a family member from a relative who had recently been in the hospital and had a diagnosis of MRSA. They also found 8,064 potential transmissions of MRSA after the hospitalization of a family member who did not have an MRSA infection.
“It is important not to over-emphasize the hospital stay risk,” Miller said. “While we identified a significant risk factor for transmission in the household and community the absolute risk remains relatively low.”
People exposed to a recently hospitalized family member with MRSA were more than 71 times, or 7000%, more likely to get an MRSA infection compared to enrollees who did not have a family member who had been hospitalized or exposed to MRSA in the previous 30 days.
Having a family member in the household who was hospitalized but did not have MRSA increased the chances of a relative getting MRSA in the month after discharge by 44%.
The more time the family member spent in the hospital, the higher the likelihood that someone in their household would get MRSA. If the patient was in the hospital for one to three days in the previous month, the chance of a relative getting MRSA increased by 34% compared to people with no recent hospitalizations in their household. If a family member was hospitalized for four to 10 days, the chances of MRSA infection in a relative were 49% higher, and with hospitalizations longer than 10 days the odds of a relative in the same household getting an infection rose by 70% to 80%.
Other factors associated with MRSA infections among household members included the number of other illnesses, prior antibiotic usage, and the presence of young children in the family.
Reference: “Hospitalizations among family members increase the risk of MRSA infection in a household” by Aaron C. Miller, Alan T. Arakkal, Daniel K. Sewell, Alberto M. Segre, Bijaya Adhikari, Philip M. Polgreen and For The CDC MInD-Healthcare Group, 7 August 2024, Infection Control & Hospital Epidemiology.
DOI: 10.1017/ice.2024.106
News
Scientists May Have Found a Secret Weapon To Stop Pancreatic Cancer Before It Starts
Researchers at Cold Spring Harbor Laboratory have found that blocking the FGFR2 and EGFR genes can stop early-stage pancreatic cancer from progressing, offering a promising path toward prevention. Pancreatic cancer is expected to become [...]
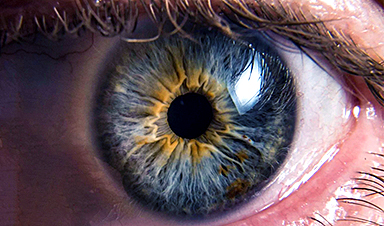
Breakthrough Drug Restores Vision: Researchers Successfully Reverse Retinal Damage
Blocking the PROX1 protein allowed KAIST researchers to regenerate damaged retinas and restore vision in mice. Vision is one of the most important human senses, yet more than 300 million people around the world are at [...]
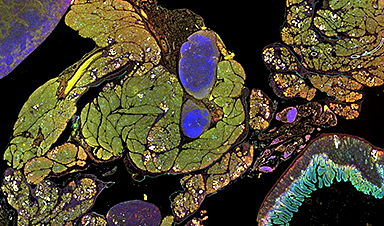
Differentiating cancerous and healthy cells through motion analysis
Researchers from Tokyo Metropolitan University have found that the motion of unlabeled cells can be used to tell whether they are cancerous or healthy. They observed malignant fibrosarcoma cells and [...]
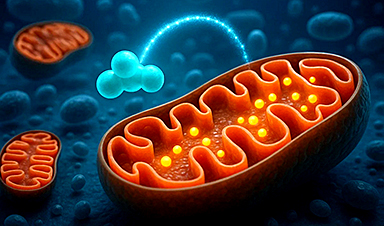
This Tiny Cellular Gate Could Be the Key to Curing Cancer – And Regrowing Hair
After more than five decades of mystery, scientists have finally unveiled the detailed structure and function of a long-theorized molecular machine in our mitochondria — the mitochondrial pyruvate carrier. This microscopic gatekeeper controls how [...]
Unlocking Vision’s Secrets: Researchers Reveal 3D Structure of Key Eye Protein
Researchers have uncovered the 3D structure of RBP3, a key protein in vision, revealing how it transports retinoids and fatty acids and how its dysfunction may lead to retinal diseases. Proteins play a critical [...]
5 Key Facts About Nanoplastics and How They Affect the Human Body
Nanoplastics are typically defined as plastic particles smaller than 1000 nanometers. These particles are increasingly being detected in human tissues: they can bypass biological barriers, accumulate in organs, and may influence health in ways [...]
Measles Is Back: Doctors Warn of Dangerous Surge Across the U.S.
Parents are encouraged to contact their pediatrician if their child has been exposed to measles or is showing symptoms. Pediatric infectious disease experts are emphasizing the critical importance of measles vaccination, as the highly [...]
AI at the Speed of Light: How Silicon Photonics Are Reinventing Hardware
A cutting-edge AI acceleration platform powered by light rather than electricity could revolutionize how AI is trained and deployed. Using photonic integrated circuits made from advanced III-V semiconductors, researchers have developed a system that vastly [...]
A Grain of Brain, 523 Million Synapses, Most Complicated Neuroscience Experiment Ever Attempted
A team of over 150 scientists has achieved what once seemed impossible: a complete wiring and activity map of a tiny section of a mammalian brain. This feat, part of the MICrONS Project, rivals [...]
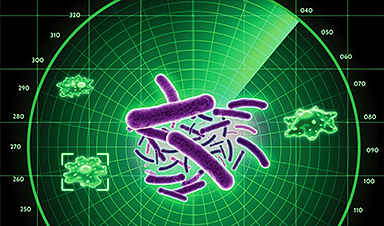
The Secret “Radar” Bacteria Use To Outsmart Their Enemies
A chemical radar allows bacteria to sense and eliminate predators. Investigating how microorganisms communicate deepens our understanding of the complex ecological interactions that shape our environment is an area of key focus for the [...]
Psychologists explore ethical issues associated with human-AI relationships
It's becoming increasingly commonplace for people to develop intimate, long-term relationships with artificial intelligence (AI) technologies. At their extreme, people have "married" their AI companions in non-legally binding ceremonies, and at least two people [...]
When You Lose Weight, Where Does It Actually Go?
Most health professionals lack a clear understanding of how body fat is lost, often subscribing to misconceptions like fat converting to energy or muscle. The truth is, fat is actually broken down into carbon [...]
How Everyday Plastics Quietly Turn Into DNA-Damaging Nanoparticles
The same unique structure that makes plastic so versatile also makes it susceptible to breaking down into harmful micro- and nanoscale particles. The world is saturated with trillions of microscopic and nanoscopic plastic particles, some smaller [...]
AI Outperforms Physicians in Real-World Urgent Care Decisions, Study Finds
The study, conducted at the virtual urgent care clinic Cedars-Sinai Connect in LA, compared recommendations given in about 500 visits of adult patients with relatively common symptoms – respiratory, urinary, eye, vaginal and dental. [...]
Challenging the Big Bang: A Multi-Singularity Origin for the Universe
In a study published in the journal Classical and Quantum Gravity, Dr. Richard Lieu, a physics professor at The University of Alabama in Huntsville (UAH), which is a part of The University of Alabama System, suggests that [...]
New drug restores vision by regenerating retinal nerves
Vision is one of the most crucial human senses, yet over 300 million people worldwide are at risk of vision loss due to various retinal diseases. While recent advancements in retinal disease treatments have [...]