When the virus hunters landed in the remote African village of Yambuku in 1976, the nuns warned them to stay back. The sisters had cordoned off the area where they were caring for people dying from a mysterious new disease. In fact, the whole village was sealed off, both by thick jungle and now quarantine – the only plane allowed in was the one carrying this special team of international doctors suddenly at their door.
“Stay back or you’ll die!” the nuns yelled.
“It’s OK, we’re here to stop the epidemic,” a young microbiologist named Peter Piot shouted back.
Weeks earlier, blood from a nun who had fallen ill with the mystery disease had arrived at his lab in Belgium, Piot recalls, with a bloodstained note from a local doctor who wondered if the mosquito-borne yellow fever could be to blame. Only this seemed even worse. Whole families succumbed, racked by uncontrollable vomiting and diarrhoea, bleeding from the eyes and mouth. When Piot helped isolate the virus from the sample, he found something entirely new. “It was big [under the] electron microscope, and long like a worm,” he says. It was Ebola.
Piot and the team soon traced its spread to unsterilised needles and the highly infectious blood of its victims. Eventually, science tracked it further back to African fruit bats and grisly outbreaks among monkeys, chimps and gorillas. As more forest was logged, and animals and humans collided, Ebola would break out again and again. But tales of how Piot and his colleagues braved the microbe to contain that first human Ebola cluster would become an epidemiological legend. “That was really the beginning of outbreak investigation,” says Piot, now the director at the London School of Hygiene and Tropical Medicine.
Today, with the world in the grip of its biggest pandemic since the 1918 flu, Bill Gates has called for a crack team of specialists to be embedded in healthcare systems around the globe, ready to contain an outbreak, as Piot and his colleagues once did. Others say we should reduce the risk of pandemics where they emerge – at the edge of the wild – by curbing logging and the wildlife trade from which both SARS and likely COVID arose.
They also say pandemics are more likely than ever. But why? And what are the best ways to stop the next one?
Where do pandemics come from?
We live on a virus planet, says Piot. There are more on Earth than stars in the sky. Fortunately, most of them can’t infect us. The few that can are mostly caught from animals – in that knife-edge moment of chance known as a “spillover” when a pathogen circulating in one species leaps to another. Some animals, such as bats, have evolved for thousands of years alongside their viruses. But as different species interact, the viruses that have grown up with one host have a chance to jump to another.
Most will fizzle out just as suddenly, but sometimes a virus will mutate into something new, even into something that can infect humans. Everything from Ebola and HIV to yellow fever, flu, and SARS began this way. “And humans can give their viruses to animals too,” says evolutionary virologist Professor Eddie Holmes, pointing to outbreaks among farmed pigs. “We’re not the end of the chain by any means.”
The wet market in Wuhan where COVID first emerged in late 2019 was the perfect place for such a spillover – and multiple studies of both the initial outbreak and COVID’s viral ancestry consistently point to it as the most likely origin of the pandemic. Holmes had been to that very market in Wuhan only five years earlier. In the south-western corner, where the fare on offer was often illegal wildlife, he’d photographed a fluffy raccoon dog (a species linked to the SARS outbreak along with civets at a wet market 20 years before).
Such wet markets are still popular throughout Asia, says Nobel-Prize-winning immunologist Professor Peter Doherty – part of an enduring preference for fresh meat over frozen. They are also notorious melting pots of disease, as stressed animals from all corners of the world are caged close together, trading unfamiliar germs, and then handled and butchered by humans. “We worry about it all the time with bird flu too,” says Doherty. “You get wild birds coming into market alongside poultry.”
Not all viruses are primed to go global, of course. “I don’t really worry about an Ebola pandemic because you need close contact [to spread it],” says Piot. “Though we have seen terrible outbreaks like in West Africa in 2014 when 11,000 died.” His eye is still firmly on influenza, which mutates fast and spreads easily. “We haven’t really had flu seasons for the past two winters [during the pandemic]. That means we’re not protected. Something could emerge and rip through.”
News
NanoMedical Brain/Cloud Interface – Explorations and Implications. A new book from Frank Boehm
New book from Frank Boehm, NanoappsMedical Inc Founder: This book explores the future hypothetical possibility that the cerebral cortex of the human brain might be seamlessly, safely, and securely connected with the Cloud via [...]
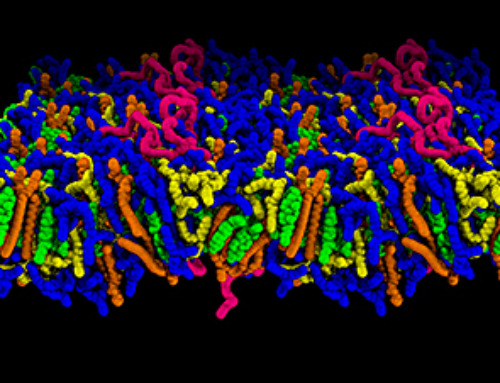
How lipid nanoparticles carrying vaccines release their cargo
A study from FAU has shown that lipid nanoparticles restructure their membrane significantly after being absorbed into a cell and ending up in an acidic environment. Vaccines and other medicines are often packed in [...]
New book from NanoappsMedical Inc – Molecular Manufacturing: The Future of Nanomedicine
This book explores the revolutionary potential of atomically precise manufacturing technologies to transform global healthcare, as well as practically every other sector across society. This forward-thinking volume examines how envisaged Factory@Home systems might enable the cost-effective [...]
A Virus Designed in the Lab Could Help Defeat Antibiotic Resistance
Scientists can now design bacteria-killing viruses from DNA, opening a faster path to fighting superbugs. Bacteriophages have been used as treatments for bacterial infections for more than a century. Interest in these viruses is rising [...]
Sleep Deprivation Triggers a Strange Brain Cleanup
When you don’t sleep enough, your brain may clean itself at the exact moment you need it to think. Most people recognize the sensation. After a night of inadequate sleep, staying focused becomes harder [...]
Lab-grown corticospinal neurons offer new models for ALS and spinal injuries
Researchers have developed a way to grow a highly specialized subset of brain nerve cells that are involved in motor neuron disease and damaged in spinal injuries. Their study, published today in eLife as the final [...]
Urgent warning over deadly ‘brain swelling’ virus amid fears it could spread globally
Airports across Asia have been put on high alert after India confirmed two cases of the deadly Nipah virus in the state of West Bengal over the past month. Thailand, Nepal and Vietnam are among the [...]
This Vaccine Stops Bird Flu Before It Reaches the Lungs
A new nasal spray vaccine could stop bird flu at the door — blocking infection, reducing spread, and helping head off the next pandemic. Since first appearing in the United States in 2014, H5N1 [...]
These two viruses may become the next public health threats, scientists say
Two emerging pathogens with animal origins—influenza D virus and canine coronavirus—have so far been quietly flying under the radar, but researchers warn conditions are ripe for the viruses to spread more widely among humans. [...]
COVID-19 viral fragments shown to target and kill specific immune cells
COVID-19 viral fragments shown to target and kill specific immune cells in UCLA-led study Clues about extreme cases and omicron’s effects come from a cross-disciplinary international research team New research shows that after the [...]
Smaller Than a Grain of Salt: Engineers Create the World’s Tiniest Wireless Brain Implant
A salt-grain-sized neural implant can record and transmit brain activity wirelessly for extended periods. Researchers at Cornell University, working with collaborators, have created an extremely small neural implant that can sit on a grain of [...]
Scientists Develop a New Way To See Inside the Human Body Using 3D Color Imaging
A newly developed imaging method blends ultrasound and photoacoustics to capture both tissue structure and blood-vessel function in 3D. By blending two powerful imaging methods, researchers from Caltech and USC have developed a new way to [...]
Brain waves could help paralyzed patients move again
People with spinal cord injuries often lose the ability to move their arms or legs. In many cases, the nerves in the limbs remain healthy, and the brain continues to function normally. The loss of [...]
Scientists Discover a New “Cleanup Hub” Inside the Human Brain
A newly identified lymphatic drainage pathway along the middle meningeal artery reveals how the human brain clears waste. How does the brain clear away waste? This task is handled by the brain’s lymphatic drainage [...]
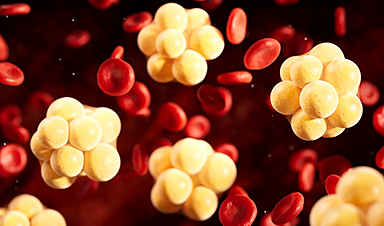
New Drug Slashes Dangerous Blood Fats by Nearly 40% in First Human Trial
Scientists have found a way to fine-tune a central fat-control pathway in the liver, reducing harmful blood triglycerides while preserving beneficial cholesterol functions. When we eat, the body turns surplus calories into molecules called [...]
A Simple Brain Scan May Help Restore Movement After Paralysis
A brain cap and smart algorithms may one day help paralyzed patients turn thought into movement—no surgery required. People with spinal cord injuries often experience partial or complete loss of movement in their arms [...]