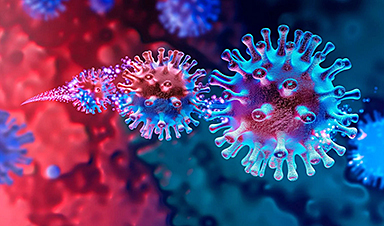
The omicron variant of the SARS-CoV-2 virus, discovered just a few weeks ago, is poised to dominate Covid-19 cases around the world. It's a stunning new twist to the pandemic saga that has countries scrambling to prepare.
In places like South Africa and the United Kingdom where omicron has been spreading fast, Covid-19 cases have doubled every three days or less. This includes people who were previously infected or vaccinated against Covid-19.
"It's the ability to evade immunity coupled with this really high transmission rate that are the two things that set this variant apart from all the rest that have come before," said Andrew Pekosz, a professor of microbiology at Johns Hopkins University.
Omicron could therefore push the Covid-19 pandemic into its worst phase yet. Or it might not. It's not yet clear whether these traits will drive up hospitalizations and deaths to record levels in the US and beyond, but epidemiological models show that omicron is likely to have a heavy toll this winter. Yet in South Africa, it appears that its omicron wave has already peaked without heavy casualties. How bad omicron gets also hinges on how people respond to it, particularly when it comes to getting vaccinated or boosted.
Researchers are now racing to understand the variant to anticipate its next moves, but it's proving to be challenging. From its genetic origins to the way it infects people, omicron is unusual and perplexing. Through studying the genetics of the variant, scientists hope to get more clues about where it came from and potentially prevent the next variant from catching the world off-guard.
The mutations in the omicron variant make it more prolific, dangerous, and elusive
There are close to 50 mutations in the omicron variant compared to the original SARS-CoV-2 virus detected in China in 2019. These changes are manifesting in several key ways.
One of the most important areas is in the spike protein of the virus. This is the part of the virus that comes into contact with human cells, and a prominent target for the immune system. Antibodies attach to the spike protein and stop the virus from causing an infection. This makes the spike protein critical for how the virus functions and for how the immune system stops it.
Omicron has 36 mutations in its spike protein, compared to 10 in alpha, 12 in gamma, and nine in delta. Within its spike protein, omicron has mutations in the part of the spike that connects directly to a receptor called ACE2 on human cells. Omicron's mutations seem to increase its affinity for ACE2, allowing it to more efficiently infect cells, thereby increasing its reproduction rate and transmissibility.
There are mutations on other parts of omicron's spike protein as well. Because of these changes, antibodies have a harder time recognizing and sticking to omicron's spike. That may explain why omicron seems to cause more reinfections and breakthrough infections in vaccinated people compared to other variants.
These changes to the spike protein also make therapies that use antibodies — monoclonal antibodies and convalescent plasma — less effective. So far, only sotrovimab, the monoclonal antibody therapy developed by GlaxoSmithKline, seems to be effective against omicron.
Other therapies like antiviral drugs should still remain as effective against omicron, since they act on how the virus replicates instead of targeting its outer structure.
But most of these drugs have to be administered in the early stages of infection, which often requires testing to confirm. The Food and Drug Administration this week granted its first emergency use authorization for an oral antiviral drug to treat Covid-19, Pfizer's Paxlovid, for high-risk patients.
Most Covid-19 vaccines are optimized to help the immune system target the SARS-CoV-2 spike protein, and the changes in omicron do seem to render the first generation of vaccines less effective. But their efficacy against omicron isn't zero, and with booster doses, protection from the variant improves dramatically. Moderna reported this week that a half-dose booster of its mRNA vaccine raised antibody levels against omicron 37-fold, while a full dose raised antibody levels 83-fold compared to just the two initial doses. That echoes a report from Pfizer that a third dose of its vaccine made it just as effective against omicron as the initial doses were against the original virus.
Researchers at the University of Hong Kong recently reported another change with omicron: where it replicates in the body. In a study that has not yet been peer-reviewed, the team found that omicron multiplies 70 times faster in the bronchi — the passages leading into the lungs — compared to delta, as soon as 24 hours after infection. But deeper in the lungs, omicron replicates at a rate lower than the original version of the virus.
In the upper airways, more virus replication may make it easier to breathe out virus particles, allowing them to spread more readily between people. And with lower numbers in the lungs, it may cause less severe illness compared to other variants.
But it's still not clear how severe of an illness omicron can cause. And even if omicron causes less severe illness, it can still dangerously stress the health system if it spreads unchecked. The fraction of people becoming severely sick may be lower, but the absolute number could be higher, filling up beds in ICUs and devouring resources that would otherwise go toward treating other conditions.
Early reports from places like South Africa and the United Kingdom showed a precipitous rise in new Covid-19 cases, but so far hospitalizations have not surged as dramatically in their wake. That could be because omicron doesn't make people as sick, but it could also be that those areas already have widespread immunity from previous waves of Covid-19 and from vaccines. Better treatment options may also be cushioning the blow.
It seems clear that omicron will become the dominant source of new Covid-19 cases in the United States as well, but whether that's followed by extreme illnesses and deaths is less certain. The holiday travel season may fuel more infections, but high levels of vaccinations and boosters in some regions could absorb the impact. In states and cities with low levels of immunity, omicron could be far more devastating. It would further widen the divide in how the pandemic is playing out across the country.
Omicron is a distant relative of other variants, but its origins are a mystery
Omicron is the latest symptom of the rampaging global Covid-19 pandemic. The world has turned into a proving ground for SARS-CoV-2, giving the virus ample opportunity to spread, evolve, test its strategies against immunity, and optimize itself. With such large disparities in vaccination rates between countries, billions of people remain unprotected, creating opportunities for more variants. And when variants infect people with waning immunity, they're spurred to change even more.
"It's Darwinian evolution by natural selection working at incredibly fast time frames," said Pekosz.
It's important to remember that viruses mutate all the time as they replicate. Most of these changes are either inconsequential or harmful to the virus itself. Occasionally a concerning mutation will arise, one that makes the virus cause more severe illness, spread more readily, or better evade the immune system. Clusters of these mutations are categorized as variants.
These variants don't spontaneously emerge; they evolve and iterate from existing versions of the virus. So by sequencing the genomes of different variants, scientists can trace their ancestry.
Scientists map out genetic relationships between variants in diagrams known as phylogenetic trees. Most of the previous variants were closer to each other genetically, but omicron isn't descended from any of them, suggesting it stems from an even earlier version of the virus. In the phylogenetic tree of SARS-CoV-2, genetic sequences of omicron (seen in red below) form their own distinct branch:
 © Nextstrain This radial phylogenetic tree of SARS-CoV-2 depicts known sequences of variants (dots) and their relationships to each other. The length of the branches indicate how divergent a given variant is. Omicron, depicted in red, stands out for its uniqueness.
© Nextstrain This radial phylogenetic tree of SARS-CoV-2 depicts known sequences of variants (dots) and their relationships to each other. The length of the branches indicate how divergent a given variant is. Omicron, depicted in red, stands out for its uniqueness.On a lone red spoke, omicron sticks out with few genome sequences connecting it back to its ancestors, almost like it appeared out of nowhere.
"It's very striking how far this variant has diverged from other variants," said Brianne Barker, an associate professor of biology at Drew University.
"What we can tell from looking at the phylogenetic tree is that this version of the virus has been in a location where it was not caught by sequencing for a long period of time," Barker added. While omicron was first reported in Botswana and South Africa, it may have been spreading elsewhere previously without anyone's knowledge.
There are a few theories for why omicron seemed to spring up suddenly. It may have been spreading all along and was missed by genetic surveillance efforts. But if that's the case, why didn't such a transmissible variant change Covid-19 patterns earlier? It's unclear.
Another possibility is that it emerged from a longer-term infection in an immunosuppressed person who didn't have a strong arsenal of B cells, T cells, and antibodies to rapidly clear out the virus. That would have given it time to acquire mutations that help it elude the immune system.
"I think the immunocompromised hypothesis is probably the most likely," Barker said. However, she noted that usually variants that arise in such cases tend to be less able to infect people with robust immune systems.
A third prospect is that omicron may have come from an animal host. Given that SARS-CoV-2 has already shown it can spread to a number of different animals — minks, bats, tigers, apes — it's not far-fetched that the virus could leap back into people. Some genetic analysis work does hint at this route, according to Barker, but animals are even less studied than humans when it comes to Covid-19. So far, no animal has been found with a virus that looks like it could have spawned omicron.
There's also the chance that omicron arose from recombination. That's when an individual is infected with two different varieties of the virus at the same time, allowing the viruses to swap parts, resulting in a new virus that has some traits from each of its parents. If that's what happened, scientists would expect to see a closer genetic relationship between omicron and the viruses it came from than what is evident in the phylogenetic tree above.
Figuring out where omicron came from may seem like an academic discussion, but it can reveal potential routes for future changes to the virus and tactics to close them off. "In any case, we're going to learn some interesting virology, but understanding the provenance of this virus can tell us some things about things we might need to do to further stop this pandemic," Barker said.
More variants will come, but we can take steps now to stop them
While omicron may be more dangerous than its relatives, there are plenty of ways to contain its destruction.
Vaccination is critical, including getting boosters. But vaccines have to be administered around the world — not just in wealthy countries — to slow the spread of omicron and limit the emergence of new variants like it.
In addition, countries need to do a better job of sequencing the genomes of positive Covid-19 cases. That can provide a critical early warning of any new mutations. "It's in places where we're not looking where these variants seem to emerge," said Pekosz.
Slowing transmission between people by wearing effective masks, social distancing, and ensuring adequate ventilation is also important. Testing for Covid-19 remains another pillar of the containment strategy to identify potentially asymptomatic cases and to commence treatment early in the course of the illness so that the medication is most effective.
None of these measures are new, but the will to enact them is fading. There are some encouraging signs that this winter may not be as devastating as the last one. However, omicron is not going to be the last major variant of SARS-CoV-2, and the steps taken to mitigate the current wave will help forestall the next one.
News
Scientists discover natural ‘brake’ that could stop harmful inflammation
Researchers at University College London (UCL) have uncovered a key mechanism that helps the body switch off inflammation—a breakthrough that could lead to new treatments for chronic diseases affecting millions worldwide. Inflammation is the [...]
A Forgotten Molecule Could Revive Failing Antifungal Drugs and Save Millions of Lives
Scientists have uncovered a way to make existing antifungal drugs work again against deadly, drug-resistant fungi. Fungal infections claim millions of lives worldwide each year, and current medical treatments are failing to keep pace. [...]
Scientists Trap Thyme’s Healing Power in Tiny Capsules
A new micro-encapsulation breakthrough could turn thyme’s powerful health benefits into safer, smarter nanodoses. Thyme extract is often praised for its wide range of health benefits, giving it a reputation as a natural medicinal [...]
Scientists Develop Spray-On Powder That Instantly Seals Life-Threatening Wounds
KAIST scientists have created a fast-acting, stable powder hemostat that stops bleeding in one second and could significantly improve survival in combat and emergency medicine. Severe blood loss remains the primary cause of death from [...]
Oceans Are Struggling To Absorb Carbon As Microplastics Flood Their Waters
New research points to an unexpected way plastic pollution may be influencing Earth’s climate system. A recent study suggests that microscopic plastic pollution is reducing the ocean’s capacity to take in carbon dioxide, a [...]
Molecular Manufacturing: The Future of Nanomedicine – New book from Frank Boehm
This book explores the revolutionary potential of atomically precise manufacturing technologies to transform global healthcare, as well as practically every other sector across society. This forward-thinking volume examines how envisaged Factory@Home systems might enable the cost-effective [...]
New Book! NanoMedical Brain/Cloud Interface – Explorations and Implications
New book from Frank Boehm, NanoappsMedical Inc Founder: This book explores the future hypothetical possibility that the cerebral cortex of the human brain might be seamlessly, safely, and securely connected with the Cloud via [...]
Global Health Care Equivalency in the Age of Nanotechnology, Nanomedicine and Artificial Intelligence
A new book by Frank Boehm, NanoappsMedical Inc. Founder. This groundbreaking volume explores the vision of a Global Health Care Equivalency (GHCE) system powered by artificial intelligence and quantum computing technologies, operating on secure [...]
Miller School Researchers Pioneer Nanovanilloid-Based Brain Cooling for Traumatic Injury
A multidisciplinary team at the University of Miami Miller School of Medicine has developed a breakthrough nanodrug platform that may prove beneficial for rapid, targeted therapeutic hypothermia after traumatic brain injury (TBI). Their work, published in ACS [...]
COVID-19 still claims more than 100,000 US lives each year
Centers for Disease Control and Prevention researchers report national estimates of 43.6 million COVID-19-associated illnesses and 101,300 deaths in the US during October 2022 to September 2023, plus 33.0 million illnesses and 100,800 deaths [...]
Nanomedicine in 2026: Experts Predict the Year Ahead
Progress in nanomedicine is almost as fast as the science is small. Over the last year, we've seen an abundance of headlines covering medical R&D at the nanoscale: polymer-coated nanoparticles targeting ovarian cancer, Albumin recruiting nanoparticles for [...]
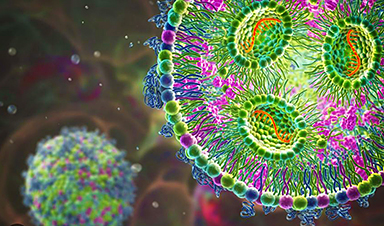
Lipid nanoparticles could unlock access for millions of autoimmune patients
Capstan Therapeutics scientists demonstrate that lipid nanoparticles can engineer CAR T cells within the body without laboratory cell manufacturing and ex vivo expansion. The method using targeted lipid nanoparticles (tLNPs) is designed to deliver [...]
The Brain’s Strange Way of Computing Could Explain Consciousness
Consciousness may emerge not from code, but from the way living brains physically compute. Discussions about consciousness often stall between two deeply rooted viewpoints. One is computational functionalism, which holds that cognition can be [...]
First breathing ‘lung-on-chip’ developed using genetically identical cells
Researchers at the Francis Crick Institute and AlveoliX have developed the first human lung-on-chip model using stem cells taken from only one person. These chips simulate breathing motions and lung disease in an individual, [...]
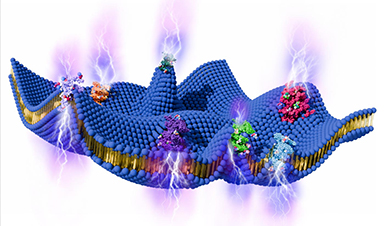
Cell Membranes May Act Like Tiny Power Generators
Living cells may generate electricity through the natural motion of their membranes. These fast electrical signals could play a role in how cells communicate and sense their surroundings. Scientists have proposed a new theoretical [...]
This Viral RNA Structure Could Lead to a Universal Antiviral Drug
Researchers identify a shared RNA-protein interaction that could lead to broad-spectrum antiviral treatments for enteroviruses. A new study from the University of Maryland, Baltimore County (UMBC), published in Nature Communications, explains how enteroviruses begin reproducing [...]